Dry Eye Disease vs Syndrome: Causes & Treatment Guide
Quick Answer: Dry eye disease and dry eye syndrome are the same condition—two interchangeable terms for when your eyes don’t produce enough quality tears to stay properly lubricated. This affects at least 16 million Americans, with women twice as likely to develop it as men. Treatment options range from simple artificial tears to advanced in-office procedures, with most people finding significant relief through personalized care.
What’s in a Name? Understanding the Terminology
Common Question: Is there a difference between dry eye disease and dry eye syndrome?
Answer: No. If you’ve been researching your eye symptoms, you’ve probably encountered both “dry eye disease” and “dry eye syndrome.” They’re in the same condition.
Both terms describe a multifactorial eye condition where your tear film doesn’t function properly, leading to discomfort and potential damage to your eye’s surface. The medical community uses these terms interchangeably, along with the technical name keratoconjunctivitis sicca (KCS).
Why the name change? The shift toward calling it “dry eye disease” reflects our deeper understanding of the condition. Rather than just a collection of symptoms (syndrome), we now recognize it as a chronic disease process involving inflammation, tear film instability, and potential long-term consequences if left untreated.
The Real Problem: When Your Tear Film Fails
Your eyes rely on a healthy tear film—a complex, three-layered protective system working constantly to keep your eyes healthy. This isn’t just about moisture; your tears perform critical functions:
- Lubricates your eye surface with every blink
- Protects against infection and environmental irritants
- Nourishes the cornea with oxygen and nutrients
- Provides a smooth optical surface for clear vision
When this system breaks down, you experience dry eye disease. The condition affects at least 16 million diagnosed Americans (approximately 6.8% of adults), though estimates suggest total cases, including undiagnosed, may reach 30-49 million. Prevalence increases significantly with age, affecting 2.7% of adults aged 18-34 and 18.6% of adults over 75.
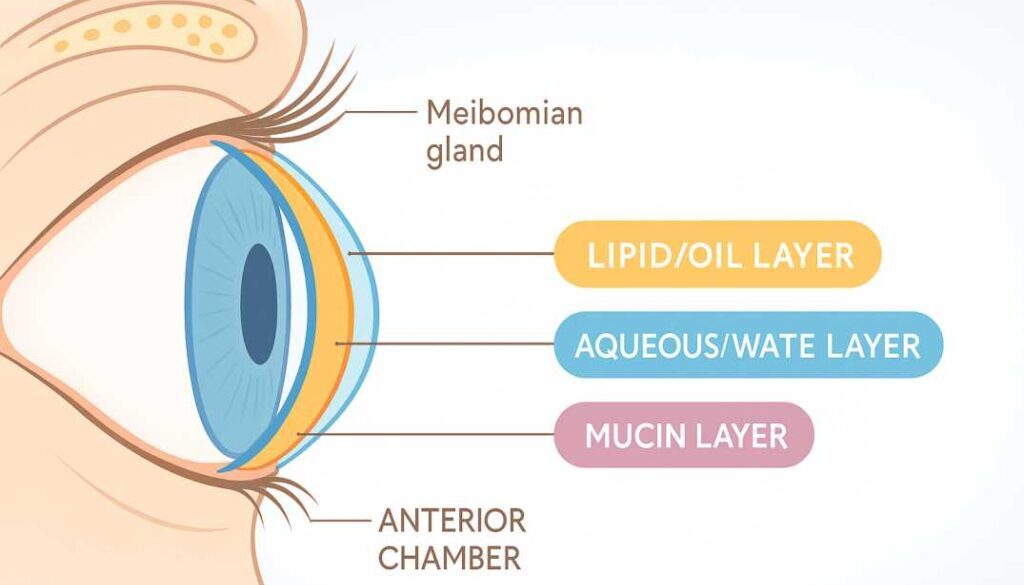
The Three Layers of Your Tear Film
-
Lipid (Oil) Layer – The outer layer produced by meibomian glands in your eyelids, preventing tears from evaporating too quickly
-
Aqueous (Water) Layer – The middle layer produced by lacrimal glands, providing moisture and washing away debris
-
Mucin Layer – The inner layer that helps tears spread evenly across your eye surface
Two Main Types of Dry Eye Disease
Understanding which type affects you is crucial for determining the most effective treatment approach.
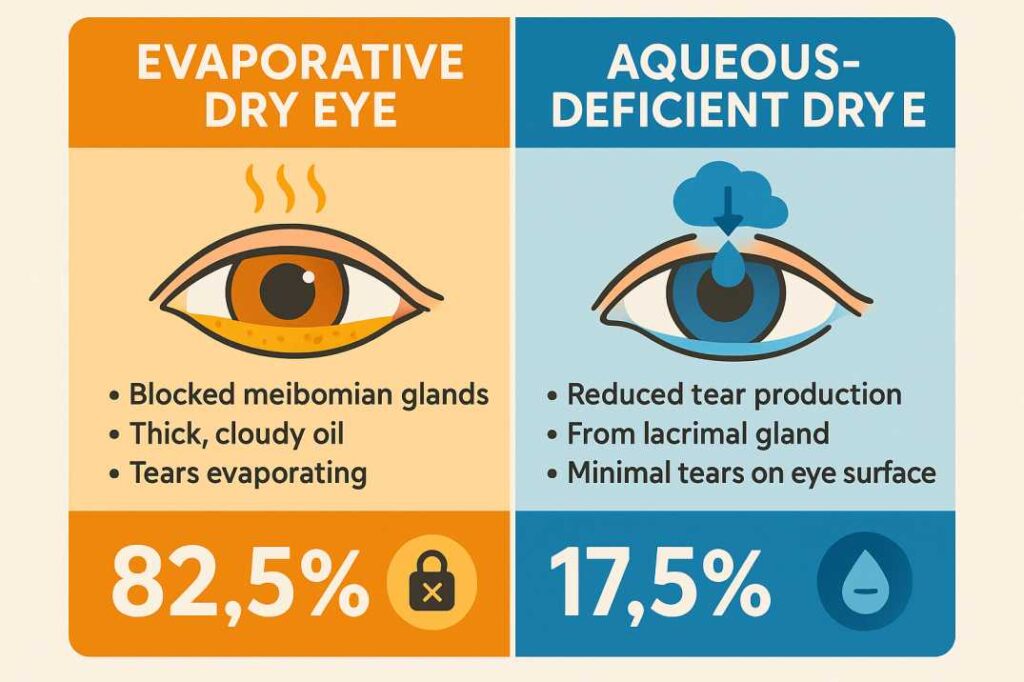
Evaporative Dry Eye (Most Common)
This type accounts for approximately 82.5% of dry eye cases and occurs when tears evaporate too quickly from your eye surface. The primary culprit? Meibomian gland dysfunction (MGD).
What is MGD? Your eyelids contain 20-30 tiny oil glands in the upper lid and 20-30 in the lower lid (meibomian glands) that produce meibum—the oily substance forming your tear film’s protective outer layer. When these glands become blocked or don’t produce quality oil, tears evaporate rapidly, leaving eyes dry and irritated.
MGD affects approximately 35.8% of people globally, with prevalence varying by population. In the U.S., estimates suggest up to 70% of people over age 60 show signs of MGD. Among dry eye patients specifically, studies show 70-86% have MGD as a contributing factor.
Common causes of evaporative dry eye:
- Blocked or dysfunctional meibomian glands
- Reduced blinking (from screen use, reading, driving)
- Eyelid problems (incomplete closure, malposition)
- Environmental factors (low humidity, air conditioning, wind)
- Certain medications (isotretinoin/Accutane, glaucoma drops)
Aqueous-Deficient Dry Eye
This type occurs when your lacrimal glands don’t produce enough of the watery layer of tears. While less common than evaporative dry eye, it can be more severe, especially when associated with autoimmune conditions.
Common causes of aqueous-deficient dry eye:
- Age-related decline in tear production
- Sjögren’s syndrome and other autoimmune diseases
- Hormonal changes (pregnancy, menopause, birth control)
- Medications (antihistamines, decongestants, antidepressants)
- Nerve damage from contact lenses or LASIK surgery
- Lacrimal gland inflammation or damage
Important note: Many people have mixed dry eye, experiencing both evaporative and aqueous-deficient components simultaneously. This is why a comprehensive evaluation by an eye care professional is essential.
Recognizing the Symptoms: More Than Just Dryness
Dry eye disease symptoms can be surprisingly varied. You might experience:
Common Symptoms
- Stinging, burning, or scratchy sensation in your eyes
- Feeling like something is stuck in your eye (foreign body sensation)
- Redness and irritation that worsen throughout the day
- Blurred vision that temporarily improves when you blink
- Eye fatigue, especially after reading or extended screen use
- Difficulty wearing contact lenses comfortably
- Light sensitivity (photophobia) in bright environments
- Stringy mucus in or around your eyes
The Paradox: Why Dry Eyes Water
One of the most confusing aspects of dry eye disease is excessive tearing. When your eyes are chronically dry, they trigger reflex tearing—a flood of emergency tears attempting to relieve irritation. However, these reflex tears are watery and lack the proper composition to fix the underlying problem. This leaves you with both watery and dry eyes simultaneously, which can be frustrating and counterintuitive.
What Causes Dry Eye Disease?
Multiple factors contribute to developing dry eye disease. Understanding your risk factors helps with prevention and management.
Age and Gender
- Tear production naturally decreases with age, particularly after age 50
- Women are at significantly higher risk—approximately twice as likely as men to develop dry eye (8.8% of women vs. 4.5% of men)
- Hormonal fluctuations during pregnancy, menopause, and when taking oral contraceptives increase women’s risk
- Among diagnosed cases, about 11.1 million are women compared to 5.3 million men
Lifestyle and Environmental Factors
- Digital device use: Prolonged screen time reduces blink rate by up to 60% (computers, smartphones, tablets)
- Contact lens wear: Can decrease oxygen to the cornea and alter tear film composition over time
- Climate and environment: Low humidity, air conditioning, heating systems, wind, smoke, and air pollution
- Diet: Deficiency in vitamin A or omega-3 fatty acids affects tear quality
- Hydration: Inadequate water intake reduces overall tear production
Medical Conditions
- Sjögren’s syndrome (10% of aqueous-deficient cases) and other autoimmune diseases
- Rheumatoid arthritis, lupus, and connective tissue disorders
- Diabetes (increases risk by 1.5-2 times)
- Thyroid disorders affecting hormone balance
- Rosacea and other skin conditions affecting the eyelids
- Parkinson’s disease (reduces blink rate significantly)
Medications That May Worsen Dry Eye
Many commonly prescribed medications can contribute to dry eye symptoms:
- Antihistamines and decongestants for allergies
- Blood pressure medications (beta-blockers, diuretics)
- Antidepressants (SSRIs, tricyclics)
- Hormone replacement therapy during menopause
- Parkinson’s disease medications (anticholinergics)
- Acne medications, especially isotretinoin (Accutane)
Other Factors
- Incomplete eyelid closure during sleep
- Previous eye surgery (LASIK, PRK, cataract surgery)
- Radiation or chemical burns to the eyes
- Chronic eye inflammation
Getting an Accurate Diagnosis
Professional diagnosis is essential because dry eye symptoms can overlap with other eye conditions like allergies, infections, or inflammation. Your eye care provider will conduct several tests during a comprehensive evaluation:
Symptom Assessment
Standardized questionnaires like the Ocular Surface Disease Index (OSDI) help quantify your symptoms and their impact on daily life.
Tear Film Evaluation
- Tear breakup time (TBUT): Measures how long tears stay on your eye surface before breaking up (normal: >10 seconds)
- Tear osmolarity: Measures tear salt concentration (elevated in dry eye)
- Schirmer test: Measures tear production using small paper strips
Eyelid and Gland Examination
- Slit lamp examination: Detailed view of your eye surface, tear film, and eyelids
- Meibography: Imaging of meibomian glands to assess function and structure
- Expression testing: Gentle pressure on eyelids to evaluate oil quality and quantity
Inflammation Assessment
- MMP-9 testing: Detects inflammatory markers in tears (InflammaDry test)
- Vital staining: Uses dyes to highlight damaged areas on the eye surface
Treatment Options: From Basic to Advanced
Dry eye disease treatment should be personalized based on your specific type, severity, and underlying causes. Most people benefit from a combination of approaches.
At-Home Care
Artificial Tears and Lubricants
The foundation of dry eye management, artificial tears are available in preserved and preservative-free formulations:
- Use preservative-free drops if applying more than 4 times daily to avoid irritation
- Gels and ointments provide longer-lasting relief but may temporarily blur vision
- Consider rewetting drops specifically designed for contact lens wearers
- Try different brands to find what works best for your eyes
Warm Compresses and Lid Hygiene
Essential for managing meibomian gland dysfunction and improving oil flow:
- Apply warm compresses for 5-10 minutes twice daily using a clean, warm washcloth
- Use gentle lid scrubs or pre-moistened lid wipes to remove debris and bacteria
- Follow with a light massage along the eyelid margin to express blocked glands
- Maintain consistency—daily treatment produces the best results
Omega-3 Fatty Acid Supplements
Clinical studies show omega-3s can improve meibomian gland function and reduce inflammation:
- Recommended dose: 1,000-2,000mg combined EPA+DHA daily
- Food sources include salmon, sardines, mackerel, walnuts, and flaxseed
- Supplements are available as fish oil, krill oil, or algae-based (vegetarian option)
- Allow 3 months to see maximum benefit—be patient and consistent
Environmental Modifications
Simple changes to your surroundings can significantly reduce dry eye symptoms:
- Use a humidifier in dry environments, especially during winter heating or air conditioning use
- Position computer screens slightly below eye level to reduce eye strain and tear evaporation
- Take regular breaks from screen time using the 20-20-20 rule: every 20 minutes, look 20 feet away for 20 seconds
- Wear wraparound sunglasses outdoors to protect from wind, dust, and UV exposure
- Avoid direct airflow from fans, heaters, or car vents aimed at your face
- Stay well-hydrated by drinking 8-10 glasses of water daily
Prescription Treatments
Anti-Inflammatory Medications
These address the inflammatory component of dry eye disease at its source:
-
Cyclosporine (Restasis, Cequa): An immunosuppressant that increases natural tear production by reducing inflammation on the ocular surface. Results typically appear after 3-6 months of consistent use.
-
Lifitegrast (Xiidra): Blocks inflammatory pathways on the ocular surface, providing relief from both signs and symptoms. Many patients notice improvement within 2-4 weeks.
-
Loteprednol (corticosteroid): A steroid eye drop for short-term use during acute inflammatory flare-ups. Typically prescribed for 2-4 weeks to quickly reduce inflammation before transitioning to longer-term treatments.
Tear Stimulation
- Varenicline nasal spray (Tyrvaya): A novel treatment approved in 2023 that stimulates natural tear production through nasal nerves. Patients use it twice daily, with many experiencing increased tearing within minutes of application.
Emerging Therapies (2024-2025)
The dry eye treatment landscape continues to evolve with promising new options:
-
Reproxalap: Targets inflammatory aldehydes that accumulate in dry eye disease. Pending FDA approval with anticipated release in 2025, this represents a new approach to upstream inflammation control.
-
Perfluorohexyloctane (Miebo): A novel tear film stabilizer approved in 2023. Unlike traditional artificial tears, this unique formulation helps prevent tear evaporation without being absorbed into the eye.
-
Acoltremon: Stimulates tear production through corneal cold receptors, mimicking the body’s natural response to environmental triggers. Currently in late-stage clinical trials.
In-Office Procedures
Thermal Pulsation Devices
These advanced treatments target meibomian gland dysfunction with controlled heat and gentle pressure:
-
LipiFlow: The FDA-approved gold standard for MGD treatment. A specialized device applies heat to the inner eyelid while pulsating the outer lid to express blocked glands. Clinical studies show sustained relief in 86% of patients, with a single 12-minute treatment providing benefits lasting 6-12 months.
-
TearCare: A wearable heating system that allows natural blinking during the 15-minute treatment session. The device maintains optimal temperature while preserving normal eye function, and then the glands are manually expressed afterward.
-
iLUX: A handheld device allowing your eye doctor to visualize and treat specific blocked glands under direct observation. This targeted approach takes about 8-12 minutes per session.
Intense Pulsed Light (IPL)
Originally developed for dermatology, IPL therapy has revolutionized dry eye treatment:
- Reduces inflammation around meibomian glands by targeting abnormal blood vessels
- Improves both gland function and tear quality with cumulative benefits over multiple sessions
- Typical treatment protocol involves 4-6 sessions spaced 2-4 weeks apart
- OptiLIGHT is currently the only FDA-approved IPL device specifically for dry eye disease
- Most patients experience noticeable improvement after the second or third treatment
Punctal Plugs
Tiny, biocompatible devices inserted into the tear ducts to help retain tears on the eye surface:
- Temporary (dissolvable) plugs last 3-6 months and are ideal for trial periods
- Semi-permanent silicone plugs can be easily removed if needed
- Best suited for aqueous-deficient dry eye rather than evaporative types
- Quick, painless office procedure taking just a few minutes
- Most patients notice immediate improvement in comfort
Demodex Treatment
For blepharitis associated with microscopic Demodex mites living in eyelash follicles:
-
Lotilaner (Xdemvy): FDA-approved anti-parasitic eye drops specifically targeting Demodex mites. Applied twice daily for 6 weeks, this prescription treatment effectively reduces mite populations.
-
Tea tree oil-based cleansers: Over-the-counter lid scrubs containing tea tree oil help control mite populations when used daily as part of a lid hygiene routine.
-
In-office lid debridement: Professional cleaning removes mite debris and biofilm from eyelid margins, often combined with other treatments.
Advanced and Surgical Options
For severe cases that don’t respond to standard treatments, additional options are available:
Autologous Serum Tears
Made from your own blood plasma, these custom eye drops contain growth factors and nutrients that promote healing:
- Reserved for severe, treatment-resistant cases not responding to conventional therapies
- Requires a blood draw, which is processed in a specialized lab to create your personalized drops
- Must be stored frozen and thawed as needed, making them less convenient than standard drops
- Highly effective for promoting healing in severe ocular surface damage
- Typically used 4-8 times daily for 3-6 months or longer
Amniotic Membrane Therapy
Derived from donated placental tissue, the amniotic membrane reduces inflammation and promotes healing:
- Cryopreserved membranes: Surgically placed on the eye surface for severe damage
- Dehydrated membranes: Applied like a contact lens, dissolving over several days
- Amniotic drops: Easier to use, applied 4 times daily for 2-4 weeks
- Particularly effective for severe ocular surface damage, corneal ulcers, or chemical burns
Surgical Interventions (Rare Cases)
Surgery is rarely needed but may be considered for specific anatomical problems:
-
Eyelid surgery: Corrects eyelid malposition (ectropion, entropion) that prevents proper eyelid closure or causes abnormal tear drainage
-
Salivary gland transplantation: For extreme cases of aqueous deficiency, especially in Sjögren’s syndrome. A minor salivary gland from the mouth is transplanted near the eye to provide moisture. This complex procedure is reserved only for the most severe cases unresponsive to all other treatments.
Recent Scientific Research: What Studies Show
Study 1: Comprehensive Quality of Life Impact (2024)
A systematic review published in Frontiers in Medicine examined how different dry eye treatments affect patient quality of life across multiple dimensions. The research analyzed treatments including artificial tears, prescription medications, thermal pulsation systems, and intense pulsed light therapy.
Key Finding: The study demonstrated that addressing the underlying cause—whether evaporative or aqueous-deficient—led to significantly better outcomes than symptom management alone. Patients who received targeted treatment based on their specific dry eye type reported improvements not just in eye comfort, but in daily activities, work productivity, and overall life satisfaction.
This research emphasizes the critical importance of proper diagnosis and personalized treatment plans that consider both objective clinical signs and subjective patient experience.
Study 2: Epidemiology and Risk Factors (2024)
A comprehensive review in Medicina analyzed dry eye disease prevalence and risk factors across diverse populations worldwide. The research synthesized data from population-based studies involving thousands of participants to provide updated estimates for 2024.
Key Finding: The study confirmed that 10-20% of the population over age 40 experiences moderate to severe dry eye symptoms. More importantly, researchers identified modifiable risk factors that patients can address: screen time (with blinking decreasing by up to 60% during device use), environmental conditions (humidity, air quality), and dietary omega-3 intake.
The study highlighted that early intervention targeting these modifiable factors can significantly reduce disease progression, making prevention just as important as treatment.
Study 3: Middle East Population Study (2024)
Published in Cureus, this meta-analysis examined dry eye prevalence across 10 Middle Eastern countries with 22,087 subjects, providing insights into how geographic and lifestyle factors influence disease rates.
Key Finding: The pooled prevalence was 28.33%, notably higher than global averages. Primary risk factors included age, female gender, smoking, prolonged screen time (over 6 hours daily), diabetes, and autoimmune diseases. Environmental factors unique to the region—including extreme heat, low humidity, and high air pollution—contributed significantly to increased prevalence.
This research demonstrates how environmental and lifestyle factors can dramatically impact dry eye disease rates, suggesting that personalized treatment must account for a patient’s specific circumstances and environmental exposures.
Prevention: Protecting Your Eyes Before Problems Start
While some risk factors like age and genetics cannot be changed, many aspects of dry eye disease are preventable through lifestyle modifications and proactive care.
Daily Habits That Protect Your Eyes
Hydration and Nutrition
- Drink 8-10 glasses of water daily to maintain adequate tear production
- Eat foods rich in omega-3 fatty acids: salmon, sardines, walnuts, flaxseed, chia seeds
- Include vitamin A sources in your diet: carrots, sweet potatoes, spinach, liver
- Limit caffeine and alcohol, which can contribute to dehydration
Screen Time Management
- Follow the 20-20-20 rule consistently: every 20 minutes, look at something 20 feet away for 20 seconds.
- Position screens slightly below eye level to reduce eye surface exposure
- Increase text size to reduce eye strain and squinting
- Use blue light filters or computer glasses if working extended hours
- Take regular breaks from digital devices, especially before bedtime
Proper Eye Care Routine
- Remove all eye makeup thoroughly before bed using gentle, oil-free cleansers
- Never sleep in contact lenses unless specifically designed for extended wear
- Replace contact lenses according to your eye doctor’s schedule
- Keep contact lens cases clean and replace them every 3 months
- Maintain good eyelid hygiene with daily gentle cleaning
Environmental Control Measures
Creating eye-friendly surroundings reduces exposure to dry eye triggers:
Indoor Environment
- Use a humidifier when heating or air conditioning systems are running, maintaining 30-50% humidity.y
- Position fans and vents away from your face and workspace
- Keep indoor temperatures moderate rather than excessively warm or cool
- Consider air purifiers to reduce dust, allergens, and irritants
Outdoor Protection
- Wear wraparound sunglasses or protective eyewear in windy, dusty, or sunny conditions
- Avoid prolonged exposure to smoke, whether from cigarettes, campfires, or pollution
- Be aware of high pollen days if you have allergies
- Protect your eyes during swimming with properly fitted goggles
Regular Eye Examinations
Preventive care catches problems early when they’re easiest to treat:
Annual Comprehensive Eye Exams Are Essential If You:
- Are over age 50 (natural tear production declines)
- Have risk factors like diabetes, autoimmune disease, or thyroid disorders
- Take medications that affect tear production
- Wear contact lenses regularly
- Have had refractive surgery (LASIK, PRK)
- Spend more than 6 hours daily on digital devices
- Have a family history of dry eye or Sjögren’s syndrome
Early detection allows for intervention before symptoms become severe, preventing long-term complications and maintaining optimal eye health throughout your life.
When to See Your Eye Doctor
Don’t wait to seek professional care if you experience:
Schedule an Appointment For:
- Persistent symptoms lasting more than a few days despite using over-the-counter treatments
- Worsening symptoms that interfere with daily activities like reading, driving, or working
- Vision changes, including blurred vision not corrected by blinking
- Eye pain or severe redness that doesn’t improve
- Discharge from the eyes (yellow, green, or crusty)
- Light sensitivity makes it difficult to be in normal lighting
- Difficulty performing activities you normally enjoy due to eye discomfort
Seek Emergency Care For:
- Sudden vision loss or significant vision changes
- Severe eye pain with light sensitivity
- Eye injury or trauma
- Signs of infection (thick discharge, swelling, fever)
- Chemical exposure to the eyes
- Foreign object stuck in the eye
Local Care: If you’re in the West Broward County area, including Tamarac, Coral Springs, or Parkland, schedule a comprehensive dry eye evaluation to determine your specific type and optimal treatment plan.
Living Well with Dry Eye Disease
Dry eye disease is a chronic condition requiring ongoing management, but with proper treatment and lifestyle adjustments, most people achieve significant relief and maintain excellent quality of life.
What to Expect from Treatment
Improvement Timeline
- Most treatments require 4-12 weeks to show their full benefits—patience and consistency are essential..
- Some therapies, such as warm compresses, provide immediate comfort, while prescription drops may take months.
- In-office procedures like IPL typically show results after 2-3 sessions over 6-8 weeks.s
- Combination therapy almost always works better than relying on a single treatment alone..
Long-Term Management
- Once symptoms improve significantly, continue preventive measures to maintain results.
- Treatment plans often need adjustments as your condition evolves or life circumstances change.
- Seasonal variations may require temporary treatment intensification (winter heating, summer air conditioning)
- Regular follow-up appointments help optimize your care and catch problems early.y
Managing Your Expectations Realistically
Understanding Treatment Goals
- Complete “cure” is rare for chronic dry eye, but excellent symptom control is achievable for most pat. ients
- The goal is a comfortable, functional vision that doesn’t interfere with your daily activities.
- Some trial and error is normal—finding the right treatment combination takes time and patience.e
- Consistent adherence to your treatment plan is crucial for long-term success.
Working with Your Eye Care Team
- Be honest about which treatments you’re actually using and any side effects you experience
- Report any changes in symptoms promptly so adjustments can be made
- Ask questions whenever something is unclear—understanding your condition empowers better self-care
- Request written instructions for complex treatment regimens to ensure proper technique
Important Questions to Ask Your Eye Doctor
Come prepared to your appointments with these essential questions:
- What type of dry eye do I have? (Evaporative, aqueous-deficient, or mixed)
- What’s causing my specific condition? (Identifying root causes helps target treatment)
- Which treatments are most appropriate for my situation? (Based on your type and severity)
- How long until I can expect noticeable improvement? (Realistic timeline for your specific treatments)
- Are any of my other medications contributing to the problem? (Many drugs affect tear production)
- Should I stop wearing contact lenses temporarily or permanently? (Depends on severity)
- What lifestyle changes would help most in my case? (Personalized recommendations)
- How often do I need follow-up appointments? (Monitoring is essential for optimal outcomes)
- What symptoms should prompt me to call before my next scheduled visit? (Warning signs to watch for)
- Are there any complications I should watch for? (Understanding risks helps prevent problems)
Resources and References
The information in this article is supported by peer-reviewed scientific research and authoritative medical sources. Below are three key studies referenced:
1. Impact of Dry Eye Disease Treatment on Patient Quality of Life (2024)
Source: Lin, C-W., Lin, M-Y., Huang, J-W., Wang, T-J., & Lin, I-C. (2024). Frontiers in Medicine, 11:1305579.
This comprehensive systematic review examined how different dry eye treatments affect patients ‘ quality of life across multiple dimensions. The study analyzed various treatment modalities, including artificial tears, prescription medications, thermal pulsation systems, and intense pulsed light therapy, providing evidence that addressing the underlying cause leads to significantly better outcomes than symptom management alone.
Access: https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2024.1305579/full
2. Epidemiology and Risk Factors of Dry Eye Disease (2024)
Source: Stapleton, F., et al. (2024). Medicina, 60(9):1458.
This review provides current knowledge on the incidence, prevalence, and risk factors of dry eye disease, emphasizing both modifiable and non-modifiable factors. The study confirms that 10-20% of the population over 40 experiences moderate to severe symptoms and identifies key risk factors, including screen time, environmental conditions, and dietary factors.
Access: https://www.mdpi.com/1648-9144/60/9/1458
3. Dry Eye Disease Prevalence ithe n the Middle East Population (2024)
Source: Mohamed, A., et al. (2024). Cureus, 16(9):e70522.
This meta-analysis examined dry eye prevalence across 10 Middle Eastern countries with 22,087 participants, revealing a pooled prevalence of 28.33%. The study identified primary risk factors, including age, female gender, prolonged screen time, diabetes, and environmental factors, demonstrating how geographic and lifestyle factors significantly impact disease prevalence.
Access: https://pmc.ncbi.nlm.nih.gov/articles/PMC11524650/
Additional Authoritative Sources
Information in this article also draws from:
- Mayo Clinic – Leading nonprofit medical center providing patient-centered health information
- National Eye Institute (NEI) – U.S. government’s principal agency for vision research
- American Academy of Ophthalmology -The world’s largest association of eye physicians and surgeons
- Cleveland Clinic – Nonprofit academic medical center recognized for clinical excellence
The Bottom Line: Taking Control of Your Eye Health
Dry eye disease and dry eye syndrome represent the same condition—a common, manageable eye health issue affecting millions of Americans. Whether your symptoms are mild or severe, understanding the causes and available treatments empowers you to take control of your eye health and find lasting relief.
Key Takeaways for Your Journey
Understanding and Diagnosis
- Early intervention prevents progression and serious complications
- A comprehensive professional evaluation identifies your specific type and underlying causes
- Accurate diagnosis is the foundation for effective, targeted treatment
Treatment and Management
- Personalized treatment combining multiple approaches typically works best
- Consistency with your treatment plan maintains comfort and protects your vision
- Most people achieve significant symptom relief with appropriate care
- Professional guidance ensures optimal outcomes and prevents trial-and-error frustration
Taking Action
- Don’t let dry eye disease diminish your quality of life—help is available
- Today’s advanced diagnostic tools and expanding treatment options offer more solutions than ever before
- Your eyes deserve expert care from professionals who understand this complex condition
- Regular follow-up appointments ensure your treatment stays effective as your needs evolve
Your Path to Relief Starts Here
With today’s comprehensive treatment options ranging from simple at-home remedies to cutting-edge in-office procedures, most people with dry eye disease find significant relief and return to comfortable, clear vision. The key is seeking professional evaluation and committing to a personalized treatment plan that addresses your specific needs.
Your vision is precious and irreplaceable. If you’re experiencing symptoms of dry eye disease—whether occasional discomfort or persistent irritation—schedule a comprehensive eye examination. Early diagnosis and proper management can prevent complications, preserve your vision, and restore the comfort you deserve.
Remember: dry eye disease is highly treatable, and you don’t have to live with the discomfort. Take the first step toward healthier, more comfortable eyes today. Symptoms are mild or severe; understanding the causes and available treatments empowers you to take control of your eye health.
The key takeaways:
- Early intervention prevents progression and complications
- A comprehensive evaluation identifies your specific type and causes
- Personalized treatment combining multiple approaches works best
- Consistent management maintains comfort and protects vision
- Professional care is essential for optimal outcomes
Don’t let dry eye disease diminish your quality of life. With today’s advanced diagnostic tools and expanding treatment options, most people find significant relief. Your eyes deserve expert care from professionals who understand the complexity of this condition and stay current with the latest treatments.
Remember, your vision is precious. If you’re experiencing symptoms of dry eye disease, schedule a comprehensive eye examination to start your journey toward comfortable, healthy eyes.
About West Broward Eyecare Associates: We provide comprehensive eye care for patients of all ages in Tamarac, Florida, and surrounding communities. Our experienced team specializes in diagnosing and treating dry eye disease using the latest technology and evidence-based approaches. Schedule your dry eye evaluation today to find lasting relief.