Dry Eye Relief FAQ | Causes, Treatments & Home Remedies in Coral Springs FL
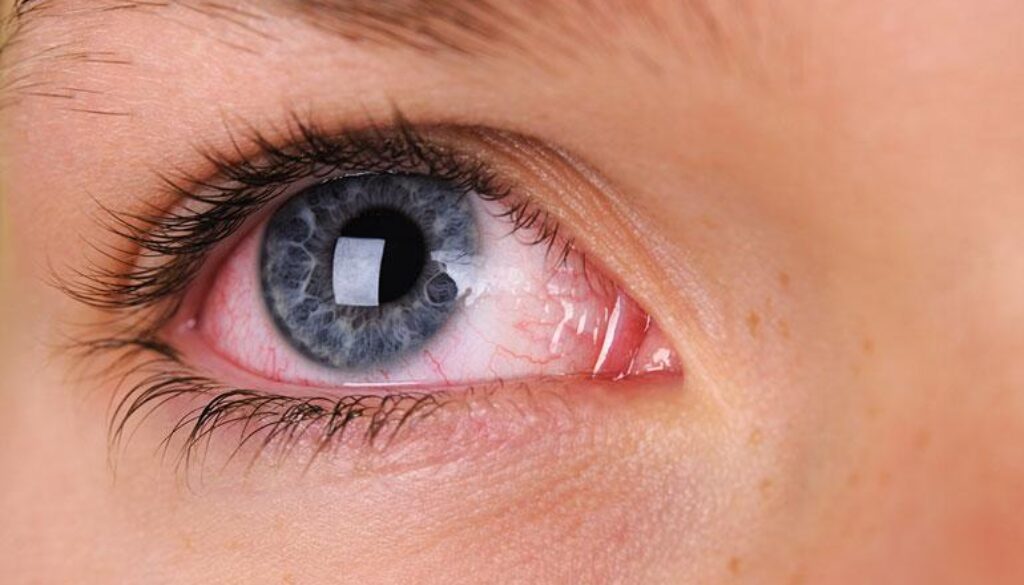
Dry eye isn’t just a minor irritation—it’s a chronic condition that can interfere with daily comfort, work, and even your mood. People often describe it as a scratchy or gritty feeling, constant burning, or a film that blurs their vision. For Florida residents dealing with year-round air conditioning, seasonal allergies, or high screen time, dry eye can be especially frustrating.
At West Broward Eye Care in Coral Springs, FL, our experienced optometrists help patients understand what causes their symptoms and find real relief. Using advanced diagnostics and individualized treatment plans, we treat the root causes of dryness—not just the discomfort.
Below, our specialists answer some of the most common questions about dry eye syndrome, its causes, and the latest treatments available.
Frequently Asked Questions
Eye Care near Coral Springs, FL
-
Dry eye can be temporary or long-term depending on what’s causing it. Environmental triggers like screen use, wind, or medication side effects may resolve with small lifestyle changes. However, chronic cases caused by meibomian gland dysfunction or autoimmune diseases like Sjögren’s syndrome require ongoing management.
Most patients experience significant relief within a few weeks of consistent treatment, but chronic cases benefit from regular follow-ups to keep symptoms under control (NIH, 2024). -
Not really. Crying produces reflex tears, which are mostly water and lack the natural oils that keep the eye’s surface protected. While tears from emotion provide short-term moisture, they often evaporate quickly and can even wash away protective oils, worsening dryness afterward. For lasting comfort, preservative-free artificial tears or moisturizing ointments are safer and more effective choices (AAO, 2023).
-
Yes. Allergies inflame the eye’s surface and disrupt the tear film, while antihistamines—though helpful for allergy symptoms—can reduce tear production. If you use oral allergy medication regularly, it’s wise to add lubricating drops or ask your doctor about a prescription eye drop that maintains moisture balance (Mayo Clinic, 2024).
-
They can. Severe dryness strains your eye muscles, which may cause eye fatigue, mild dizziness, or tension headaches. This happens when the eyes work harder to maintain focus through fluctuating tear layers. Addressing the underlying cause—like oil gland blockage or incomplete blinking—usually resolves the issue and prevents eye strain (Johns Hopkins Medicine, 2023).
-
Recently approved treatments like Tyrvaya® (varenicline nasal spray) stimulate tear production through the nasal nerves that signal the tear glands. It’s particularly useful for patients whose dryness stems from autoimmune disease or nerve dysfunction. It’s a gentle, non-invasive option that can complement other therapies like artificial tears or warm compresses (FDA.gov, 2022).
-
Yes. Nutrition plays a key role in tear quality.
- Omega-3 fatty acids (found in salmon, flaxseed, or supplements) support healthy oil production.
- Vitamin A (carrots, spinach, sweet potatoes) aids the surface cells of the eye.
- Hydration helps maintain tear balance.
Avoid excessive caffeine, alcohol, and salty foods—they can dehydrate you and worsen dryness (Harvard Health, 2023).
-
There’s no strong clinical evidence that castor oil effectively treats styes or dry eye. Warm compresses and prescribed antibiotic ointments are safer, proven options. DIY oil remedies can block glands or introduce bacteria, which may worsen symptoms. Always consult a licensed optometrist before trying home treatments (AAO, 2023).
-
Some home methods can help reduce discomfort between visits. For example:
- Warm compresses applied for 10 minutes can unclog oil glands.
- Humidifiers add moisture to indoor air, especially useful in homes with constant air conditioning.
- Blinking exercises during computer use improve tear distribution.
These steps support medical treatment but don’t replace a professional care plan (Cleveland Clinic, 2023).
-
Yes. Several common medications—including antihistamines, decongestants, acne medications like isotretinoin, and some antidepressants—can reduce tear production. If you suspect your prescription is contributing to dryness, don’t stop taking it on your own; instead, speak with your doctor about adjustments or supportive care options (NIH, 2024).
-
Sometimes. Severe dryness can create temporary fluctuations in pressure readings or blur vision, mimicking glaucoma. Proper diagnostic testing—like measuring corneal thickness and tear stability—helps distinguish between the two. Regular eye exams ensure accurate readings and early detection of both conditions (AAO, 2024).
-
Yes. Heat therapy is one of the simplest, most effective home treatments for dry eyes caused by oil gland dysfunction. Using a clean, microwavable eye mask for 10 minutes daily softens gland blockages and restores healthy oil flow. Follow with gentle eyelid massage for best results (BJO, 2023).
-
Most patients feel immediate relief after applying preservative-free artificial tears. However, true healing of the tear film can take two to four weeks of consistent use. Severe cases may need prescription drops or in-office therapies to stabilize the ocular surface long-term (NIH, 2024).
-
Yes. Supplements containing omega-3s, vitamin D, and vitamin B12 can reduce inflammation and improve tear quality. If you suspect a deficiency, a blood test can guide personalized supplementation. This approach supports other medical treatments and promotes overall ocular wellness (PubMed, 2023).
-
Prevention is just as important as treatment:
- Follow the 20-20-20 rule: every 20 minutes, look 20 feet away for 20 seconds.
- Keep indoor humidity between 40–60%.
- Stay hydrated and limit caffeine.
- Protect your eyes outdoors with wraparound sunglasses.
- For contact lens wearers, switch to daily disposables and avoid sleeping in your lenses.
These small steps go a long way toward protecting tear quality and preventing chronic irritation (AAO, 2023).
-
You should see a specialist if:
- Over-the-counter drops aren’t working
- Your eyes feel constantly gritty or blurred
- You wear contacts that are increasingly uncomfortable
- You have autoimmune disease, diabetes, or a history of eye surgery
At West Broward Eye Care, our doctors use diagnostic imaging to examine tear layers, gland health, and eye surface inflammation. With a personalized treatment plan, we help you regain comfort, clarity, and control over your eye health.
Final Thoughts
Dry eye isn’t a one-size-fits-all problem—and it doesn’t have to take over your life. Understanding your symptoms, nutrition, and environment makes all the difference. Whether your dryness stems from long screen hours, medications, or hormonal changes, the team at West Broward Eye Care in Coral Springs provides science-backed, compassionate solutions.
If you’re ready for relief, schedule your dry eye evaluation today and take the first step toward clearer, more comfortable vision.
OFFICE HOURS
Monday-Thursday: 9am–5pm – Friday: 9am–4pm
Saturday: closed – Sunday: closed
OUR LOCATION
7822 N. University Dr., Tamarac, FL 33321 – info@wbeca.com
Office Phone: (954) 726-0204 – Fax: (954)7211578