Wet vs Dry AMD: Types, Symptoms & Treatment Guide
Understanding Macular Degeneration: Wet vs. Dry AMD and Modern Treatment Approaches
Age-related macular degeneration represents one of the most significant threats to vision in adults over 50. As your trusted eye care partners in Tamarac and West Broward County, we understand the worry that comes with hearing this diagnosis. The good news? Understanding the condition and catching it early can make all the difference in preserving your precious sight.
Whether you’ve recently been diagnosed, have concerns about your family history, or simply want to protect your vision as you age, this comprehensive guide will walk you through everything you need to know about macular degeneration—from the differences between wet and dry types to the latest treatment breakthroughs in 2025.
What Is Macular Degeneration? Understanding the Basics
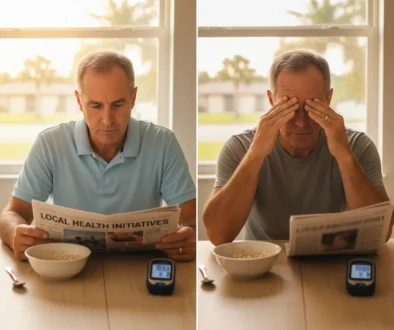
Imagine trying to read this page if the center of your vision became blurry or distorted. That’s what happens with age-related macular degeneration, commonly called AMD. This progressive eye condition damages the macula—a tiny but crucial area at the center of your retina responsible for the sharp, detailed vision you need for reading, recognizing faces, and driving.
The macula is your vision’s “sweet spot.” While peripheral vision remains intact with AMD, the central area that allows you to see fine details gradually deteriorates. Think of it like having a camera with a damaged lens center—the edges of the photo are clear, but the middle section becomes increasingly blurred or distorted.
Why “age-related“? While the exact cause isn’t fully understood, aging is the primary risk factor. The condition typically develops after age 50 and becomes increasingly common in people over 65. Currently, about 20 million Americans over 40 live with some form of macular degeneration, making it the leading cause of vision loss in older adults.
Here’s what matters most: AMD doesn’t cause complete blindness. You won’t lose all your vision, but the loss of central vision can significantly impact daily activities like reading, cooking, or driving. That’s why early detection and proper management are so critical.
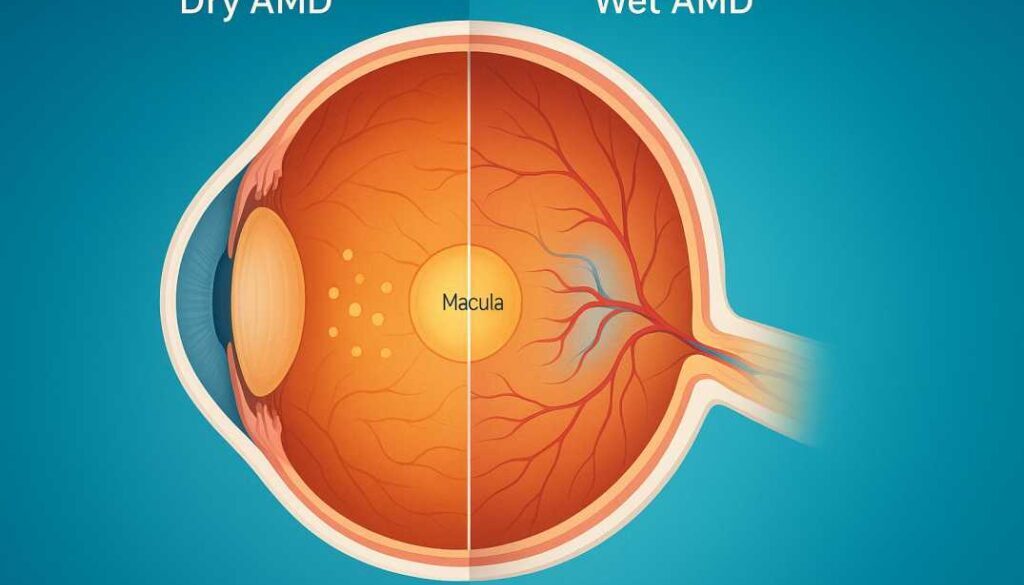
The Two Types of Macular Degeneration: Wet vs. Dry AMD
Not all macular degeneration is the same. Understanding whether you have wet or dry AMD determines your treatment path and what to expect. Let’s break down each type in clear, simple terms.
Dry AMD (Atrophic Macular Degeneration): The More Common Form
Dry AMD accounts for approximately 90% of all cases. If you’ve been diagnosed with macular degeneration, chances are high that it’s the dry type. This form develops gradually, often over years, making it easier to manage if caught early.
How Dry AMD Develops
The dry form begins when tiny yellow deposits called drusen accumulate under your macula. Think of drusen as cellular waste products—like debris that builds up over time. As these deposits increase, they can cause the macula to thin and dry out, eventually leading to damage to the light-sensing cells.
Dry AMD progresses through three distinct stages:
- Early Stage: Your eye doctor can see drusen during an exam, but you won’t notice any vision changes. Many people have early dry AMD without realizing it, which is exactly why regular eye exams after 50 are so important.
- Intermediate Stage: Drusen become larger and more numerous. You might start noticing subtle changes—perhaps needing more light to read or experiencing mild blurriness in your central vision.
- Advanced Stage (Geographic Atrophy): The macula becomes significantly thinned, and central vision loss occurs. This is the stage we work hard to prevent through early intervention.
The silver lining: Not everyone with dry AMD progresses to advanced stages. Many patients stabilize at the early or intermediate stage, especially with proper management and lifestyle changes. Vision loss tends to occur gradually, giving us time to implement protective strategies.
Wet AMD (Neovascular or Exudative AMD): The More Aggressive Form
Wet AMD represents only about 10% of cases but is responsible for the majority of severe vision loss from macular degeneration. While less common, wet AMD demands immediate attention and treatment.
How Wet AMD Develops
Wet AMD occurs when your body attempts to “fix” the damage from dry AMD by growing new blood vessels under the retina. Unfortunately, these vessels are abnormal and fragile—they leak fluid and blood into the macula, causing rapid damage and swelling.
The term “wet” refers to this fluid leakage. Unlike dry AMD’s gradual progression, wet AMD can cause sudden and dramatic vision changes. You might wake up one morning and notice straight lines appear wavy, or a dark spot may appear in your central vision seemingly overnight.
Important to know: Dry AMD can convert to wet AMD at any stage, though it’s more common in intermediate and advanced dry AMD. About 10-15% of people with dry AMD will develop the wet form. This is why ongoing monitoring is essential—catching the conversion early dramatically improves treatment outcomes.
Can You Have Both Types?
Yes, absolutely. In fact, it’s quite common. You might have dry AMD in both eyes and then develop wet AMD in one eye. Or you could have different stages in each eye—perhaps intermediate dry AMD in your right eye and wet AMD in your left. This is why we examine both eyes thoroughly and monitor each one individually.
Recognizing the Warning Signs: Symptoms of Macular Degeneration
One of the most challenging aspects of macular degeneration is that early stages often have no symptoms. You might have early dry AMD right now and not know it. That’s exactly why we recommend comprehensive eye exams starting at age 40 if you have risk factors, and annually after age 55 for everyone.
However, as the condition progresses, specific warning signs emerge:
Early and Intermediate Stage Symptoms
- Mild central blurriness that comes and goes or gradually worsens
- Difficulty seeing in low light, especially when moving from bright to dimly lit spaces
- Need for brighter light when reading or doing detailed work
- Colors appearing less vibrant or washed out
Advanced Stage Symptoms (Wet AMD or Late Dry AMD)
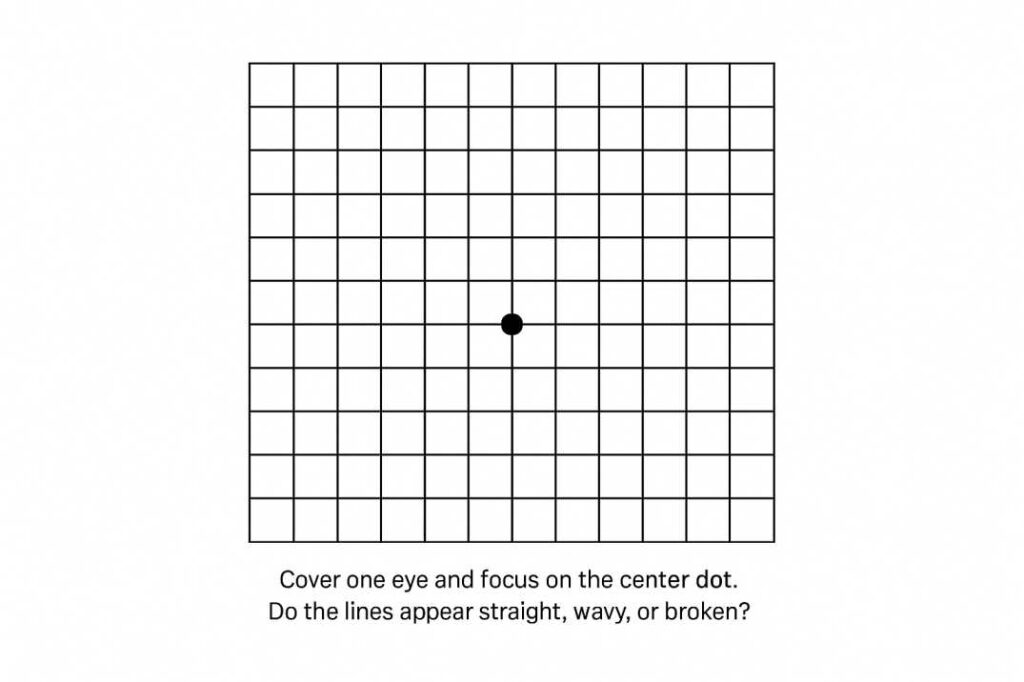
- Straight lines appearing wavy or distorted (THIS IS A RED FLAG—call your eye doctor immediately if you notice this)
- Dark or blank spots in central vision, making it hard to see faces or read
- Difficulty recognizing faces from across the room
- Objects appear in different sizes when viewed with each eye separately
The Amsler Grid Test: Your At-Home Monitoring Tool
If you have macular degeneration or are at risk, we’ll give you an Amsler grid—a simple chart with a grid of lines and a dot in the center. Test each eye separately daily. If any lines appear wavy, broken, or distorted, contact us immediately. This simple test can catch the progression from dry to wet AMD before significant damage occurs.
Who’s at Risk? Understanding Macular Degeneration Risk Factors
While anyone can develop AMD, certain factors significantly increase your risk. Understanding these can help you take proactive steps to protect your vision.
Risk Factors You Can’t Change
- Age: The single biggest risk factor. AMD is rare before 55 but increasingly common after 65. By age 80, nearly 15% of people have some form of AMD.
- Family History: Having a first-degree relative (parent, sibling) with AMD increases your risk by 3-6 times. If your family has a history, start regular screenings at age 40.
- Race: Caucasians have higher AMD rates than African Americans or Hispanics, though the condition affects all ethnic groups.
Risk Factors You Can Control
- Smoking: The most significant modifiable risk factor. Smokers have 2-3 times higher AMD risk. The good news? Quitting reduces risk within just a few years.
- Cardiovascular Disease: High blood pressure, high cholesterol, and heart disease increase AMD risk. What’s good for your heart is good for your eyes.
- Obesity: Being overweight doubles your risk of progressing from early to advanced AMD.
- Poor Diet: Diets high in saturated fats and low in antioxidants and omega-3 fatty acids increase risk.
- Sun Exposure: Chronic unprotected UV exposure may contribute to AMD development. Always wear UV-protective sunglasses outdoors.
Treatment Approaches: Modern Solutions for Protecting Your Vision
The landscape of macular degeneration treatment has transformed dramatically over the past two decades. While we still don’t have a cure, we now have powerful tools to slow progression, preserve vision, and in some cases, even improve sight. The treatment approach depends entirely on which type of AMD you have and its stage.
Managing Dry AMD: Lifestyle and Nutritional Approaches
For early and intermediate dry AMD, our primary goal is to prevent progression. While no medication currently treats early dry AMD, we have strong evidence that specific interventions can slow the disease significantly.
The AREDS2 Formula: Scientifically Proven Protection
The game-changer in dry AMD management is the AREDS2 vitamin formula. Two landmark clinical trials conducted by the National Eye Institute—AREDS (1992-2001) and AREDS2 (2006-2012)—demonstrated that specific nutritional supplements can reduce the risk of progression to advanced AMD by about 25%.
Even more encouraging, a 2024 study published in Ophthalmology revealed that AREDS2 supplements can slow vision loss in geographic atrophy (advanced dry AMD) by approximately 55% over three years. This finding has changed how we approach even late-stage dry AMD.
The AREDS2 formula includes:
- 500 mg Vitamin C
- 400 IU Vitamin E
- 10 mg Lutein
- 2 mg Zeaxanthin
- 80 mg Zinc (as zinc oxide)
- 2 mg Copper (as cupric oxide, to prevent zinc-related copper deficiency)
Critical note for smokers: The original AREDS formula contained beta-carotene, which increases lung cancer risk in current and former smokers. AREDS2 replaced beta-carotene with lutein and zeaxanthin, making it safer for everyone. If you smoke or have smoked, always choose the AREDS2 formula (without beta-carotene).
The Mediterranean Diet Connection
Research shows that following a Mediterranean diet—rich in vegetables, fruits, fish, nuts, legumes, and olive oil while limiting red meat and refined carbs—reduces AMD progression risk by 25-30%. Combined with AREDS2 supplements, this dietary approach provides comprehensive nutritional protection for your macula.
Breakthrough Treatments for Geographic Atrophy (2025 Update)
For the first time, we now have FDA-approved treatments specifically for geographic atrophy, the advanced stage of dry AMD. Two complement inhibitor medications—Syfovre (pegcetacoplan) and Izervay (avacincaptad pegol)—were approved in 2023-2024 for reducing GA growth. These medications are administered through regular eye injections and work by reducing inflammation that contributes to retinal cell death.
Additionally, photobiomodulation therapy—a non-invasive light therapy—received FDA authorization in 2025 as the first non-invasive treatment for dry AMD. This treatment uses specific wavelengths of light to stimulate cellular repair and reduce inflammation, showing promising results in clinical trials.
Treating Wet AMD: Anti-VEGF Therapy and Beyond
The treatment of wet AMD has been one of modern ophthalmology’s greatest success stories. When we catch wet AMD early and treat it consistently, we can stabilize vision in about 90% of patients and actually improve vision in 30-40% of cases. These are remarkable outcomes compared to just 20 years ago, when wet AMD almost always led to severe vision loss.
Anti-VEGF Injections: The Gold Standard Treatment
The cornerstone of wet AMD treatment is anti-VEGF (vascular endothelial growth factor) therapy. These medications block the protein that stimulates abnormal blood vessel growth under your retina. By stopping this growth, we prevent further leakage and allow existing fluid to be absorbed.
Common anti-VEGF medications include:
- Eylea (aflibercept): Can be given every 8 weeks after initial loading doses
- Lucentis (ranibizumab): Typically given monthly or as-needed based on disease activity
- Avastin (bevacizumab): Used off-label, often more cost-effective with similar efficacy
- Vabysmo (faricimab): The newest option, approved in 2022, can be given as infrequently as every 16 weeks for some patients
What to expect: Injections are performed in our office after numbing drops make the procedure comfortable. Most patients describe feeling only slight pressure. The entire process takes just a few minutes. Initially, you’ll need injections monthly for 3-4 months, then the frequency often extends based on how your eyes respond.
Emerging Gene Therapies: The Future of Wet AMD Treatment
One of the most exciting developments in 2025 is gene therapy for wet AMD. Multiple treatments are now in Phase 3 clinical trials, including RGX-314 and ADVM-022. These one-time treatments instruct your eye cells to continuously produce anti-VEGF proteins, potentially eliminating the need for frequent injections for years.
Early trial results show that many patients remain injection-free for 1-3 years after a single gene therapy treatment. While not yet FDA-approved, these therapies could revolutionize wet AMD management within the next 2-3 years.
The Port Delivery System: Long-Acting Treatment
Another innovation is Genentech’s Susvimo (port delivery system)—a permanent, refillable implant about the size of a grain of rice that continuously delivers anti-VEGF medication to your retina. Approved in the U.S., it can extend treatment intervals to every 6 months for refills, dramatically reducing treatment burden compared to monthly injections.
Living Well with Macular Degeneration: Practical Strategies
Being diagnosed with macular degeneration doesn’t mean giving up your independence or quality of life. With proper management, support, and adaptive strategies, most people with AMD continue doing the activities they love.
Low Vision Rehabilitation and Assistive Technology
If AMD has affected your central vision, low vision rehabilitation can be life-changing. Specialists teach you techniques and provide devices to maximize your remaining vision. Options include:
- Magnifying devices for reading
- Enhanced lighting systems
- Large-print materials and books
- Audio books and screen readers
- Smartphone apps with voice assistance and magnification
The Importance of Regular Eye Exams
We cannot stress this enough: regular monitoring is your best defense against vision loss from AMD. If you have early dry AMD, we’ll see you every 6-12 months. If you have intermediate AMD or are being treated for wet AMD, visits will be more frequent. This consistent monitoring allows us to catch any progression immediately when treatment is most effective.
Prevention: Protecting Your Vision for the Future
While you can’t prevent AMD entirely, you can significantly reduce your risk and slow its progression:
- Don’t smoke (or quit if you do)—this single change has the biggest impact
- Eat a nutrient-rich diet high in leafy greens, fish, and colorful fruits
- Exercise regularly to maintain cardiovascular health
- Control blood pressure and cholesterol
- Wear UV-protective sunglasses outdoors
- Maintain a healthy weight
- Get comprehensive eye exams annually after age 55 (or earlier if you have risk factors)
When to Seek Immediate Care
Call your eye doctor immediately if you experience:
- Sudden changes in vision
- Straight lines appear wavy
- Dark spots in your central vision
- Any distortion on your Amsler grid
Scientific References
This article is based on peer-reviewed research and authoritative medical sources:
- Age-Related Eye Disease Study 2 Research Group. (2013). “Lutein + zeaxanthin and omega-3 fatty acids for age-related macular degeneration: the Age-Related Eye Disease Study 2 (AREDS2) randomized clinical trial.” JAMA, 309(19), 2005-15. https://jamanetwork.com/journals/jama/fullarticle/1684847
- Keenan, T.D.L., et al. (2024). “An Updated Simplified Severity Scale for Age-Related Macular Degeneration Incorporating Reticular Pseudodrusen: Age-Related Eye Disease Study Report Number 42.” Ophthalmology, 131(10), 1164-1174. This 2024 study confirmed that AREDS2 supplements can slow geographic atrophy progression by approximately 55% over three years.
- National Eye Institute. (2025). “Age-Related Macular Degeneration (AMD).” https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/age-related-macular-degeneration. Comprehensive resource on AMD epidemiology, symptoms, and current treatment standards.
Additional research sources consulted include BrightFocus Foundation, American Academy of Ophthalmology, Cleveland Clinic, and the Macular Disease Foundation Australia.
Your Vision, Our Commitment: West Broward Eyecare’s Approach
At West Broward Eyecare Associates, we’ve seen firsthand how macular degeneration affects not just vision, but daily life, independence, and confidence. That’s why we take a comprehensive, compassionate approach to AMD care—combining cutting-edge diagnostic technology with the personalized attention your family deserves.
Whether you’re concerned about your risk, have just been diagnosed, or are managing existing AMD, we’re here to partner with you every step of the way. From advanced OCT imaging that detects the earliest changes to the latest treatment options, including anti-VEGF therapy and nutritional counseling, we provide complete AMD care right here in Tamarac.
Remember: Early detection and consistent management make all the difference. Macular degeneration is highly manageable when caught early. Don’t wait until you notice vision changes—by then, precious time may have been lost.
Schedule your comprehensive eye exam today. Your vision is worth protecting, and we’re here to help you see clearly for years to come.
Contact West Broward Eyecare Associates
Serving Tamarac, Coral Springs, Parkland, and West Broward County
Comprehensive Eye Care | Advanced AMD Diagnosis & Treatment | Family-Focused Service
FAQs
-
-
Dry AMD is more common and progresses slowly. Wet AMD is less common, more severe, with abnormal blood vessel growth causing faster vision loss.
-