Eye Inflammation & Systemic Disease Care | Rheumatoid Arthritis
Inflammation is vital for healing, but when excessive, it triggers chronic diseases like arthritis and lupus. Eye symptoms—redness, pain, blurred vision—can signal systemic inflammation, urging prompt medical evaluation.
Key Takeaways
-
Eye Symptoms Signal Systemic Issues: Redness, pain, or blurred vision may indicate inflammatory diseases like lupus or arthritis.
-
Early Detection Saves Vision: Tamarac patients with autoimmune conditions or over age 40 need routine exams using advanced OCT imaging.
-
Tailored Treatments Available: Options include steroid drops, biologics, and referrals to South Florida specialists for complex cases.
-
Lifestyle Adjustments Reduce Risk: Anti-inflammatory diets, stress management, and smoking cessation help curb inflammation.
-
Pediatric Vigilance Critical: Children with juvenile arthritis require yearly exams to detect silent, vision-threatening uveitis.
-
Innovative Diagnostics: AI imaging and tear biomarker testing enable non-invasive, precise detection of inflammation.
-
Urgent Action Prevents Vision Loss: Prompt evaluation by Dr. Rhue, an FAAO-certified expert, ensures timely care for Tamarac residents.
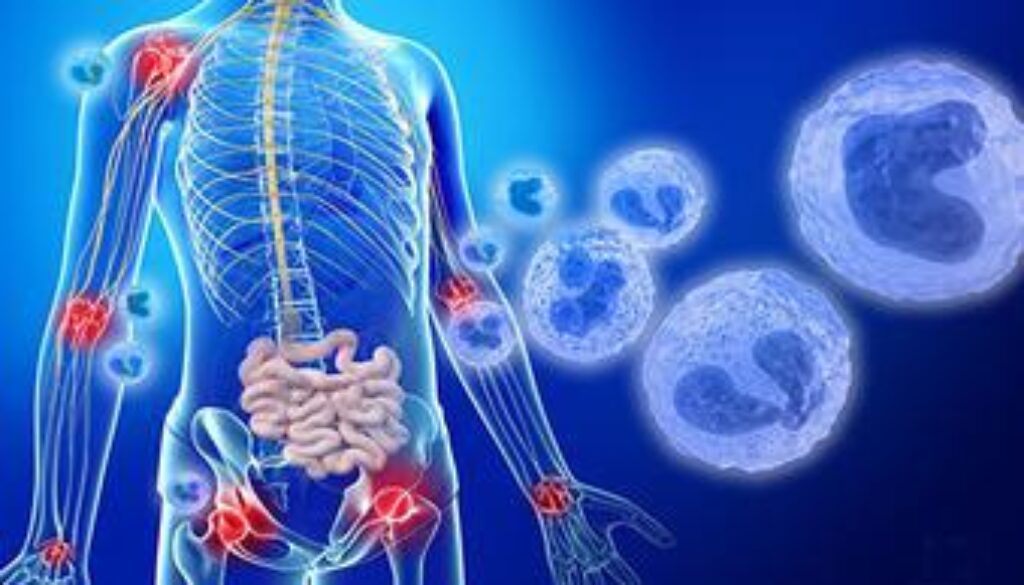
RA Eye Inflammation in Tamarac: Decoding Immune Pathways
Rheumatoid arthritis (RA) isn’t just a joint disease. At our Tamarac clinic, we see how this autoimmune condition triggers eye inflammation when misguided immune cells attack ocular tissues. Understanding these pathways helps Tamarac patients recognize early symptoms and protect their vision.
How RA Damages Eyes: The Immune Cascade
-
Autoimmune Targeting
T-cells/B-cells attack ocular structures → scleritis and tear gland inflammation. -
Cytokine Storms
TNF-α, IL-1, and IL-6 proteins fuel tissue damage, and chronic inflammation -
T-Cell Assault
TH1/TH17 cells release inflammatory signals that perpetuate the damage -
Tear System Breakdown
Lacrimal gland damage → severe dry eye (keratoconjunctivitis sicca)
Common RA Eye Conditions We Treat in Tamarac:
-
Vision-Threatening Dry Eye
Reduced tear production with inflammatory components -
Scleral Inflammation
Episcleritis (mild) vs. scleritis (severe pain/redness) -
Corneal Emergencies
Peripheral ulcerative keratitis requiring immediate intervention
RA Eye Complications: Protecting Tamarac Patients from Vision Loss
Up to 30% of rheumatoid arthritis patients develop eye complications. At our Tamarac clinic, early detection prevents irreversible damage. Recognize these common RA-related conditions:
Critical Eye Conditions We Manage:
-
RA Dry Eye (Keratoconjunctivitis Sicca)
-
Symptoms: Gritty “sand-in-eyes” sensation, burning, blurred vision
-
Cause: Immune destruction of tear glands → Inadequate eye lubrication
-
Tamarac Risk: Air conditioning and heat accelerate corneal damage
-
Urgency: Untreated cases risk corneal ulcers within 6-12 months
-
-
Episcleritis (Moderate Inflammation)
-
Symptoms: Intermittent redness, mild irritation
-
Clinical Insight: Often signals active systemic inflammation
-
Action Plan: Requires inflammation blood testing
-
-
Vision-Threatening Scleritis
-
Symptoms: Severe deep-red pain, light sensitivity, potential vision loss
-
Difference: 5x more painful than episcleritis with scleral thinning
-
Emergency Protocol: Same-day steroid treatment is available
-
-
Peripheral Ulcerative Keratitis (PUK)
-
Symptoms: Corneal edge ulcers with extreme pain/redness
-
Triage Standard: Immediate referral to our corneal specialist
-
Prognosis: 48-hour window to prevent permanent scarring
-
What does your doctor see?
- Episcleritis or Scleritis: one or more episodes of red eyes related to inflammation (not infection) could be associated with a systemic inflammatory condition
- Uveitis: inflammation of the front and or back of the eye, often associated with pain and light sensitivity
- Retinal findings: these can include inflammation surrounding the blood vessels that supply the retina or inflammatory cells within the vitreous gel of the eye
What to do if you have some of these symptoms?
Make sure to visit your optometrist to have your eyes evaluated. It is important to rule out many other causes of red eyes, blurry vision, and pain in the eyes. If your doctor suspects a systemic inflammatory cause, they may send a letter to your primary care doctor or a rheumatologist for additional blood work or work-up to rule out potential causes.
Preventive Care & Proactive Monitoring
For Tamarac residents at risk of inflammatory diseases (e.g., family history of lupus or rheumatoid arthritis), routine eye exams at West Broward Eyecare Associates are critical. Many conditions, like uveitis or scleritis, can develop silently before symptoms arise. Our Tamarac eye care team uses advanced imaging tools like optical coherence tomography (OCT) to detect subtle retinal inflammation or blood vessel changes invisible to the naked eye.
-
Who should prioritize monitoring?
-
Patients with autoimmune diagnoses (e.g., Crohn’s disease, JIA).
-
Those with unexplained joint pain or chronic fatigue (common in early-stage inflammation).
-
For adults over 40, as age increases, systemic disease risk.
-
-
How often?
-
Annual exams for high-risk patients.
-
Every 6 months if inflammation is previously detected.
Why trust us? Dr. Brianna Rhue, FAAO Board Certified Optometric Physician, partners with Tamarac rheumatologists to coordinate care, ensuring inflammation is managed holistically.
-
Treatment Pathways for Ocular Inflammation
When eye inflammation strikes, West Broward Eyecare Associates offers evidence-based treatments to protect vision and calm systemic flares:
-
Localized Therapies: Prescription steroid drops or injections to target anterior uveitis.
-
Systemic Solutions: Collaborate with Tamarac rheumatologists to prescribe biologics (e.g., Humira) for stubborn posterior uveitis or scleritis.
-
Surgical Referrals: For rare cases (e.g., retinal detachment), we connect patients with trusted South Florida specialists.
Long-term success: Our Tamarac team creates personalized plans to reduce flare-ups, combining medication adjustments and follow-up exams.
Lifestyle & Holistic Strategies to Curb Inflammation
Complement medical treatments with daily habits proven to reduce inflammation:
-
Anti-inflammatory Diets: Explore farmer’s markets in Tamarac for leafy greens, berries, and fatty fish rich in omega-3s.
-
Stress Management: Try yoga classes at Tamarac Community Center to lower cortisol.
-
Quit Smoking: Broward County’s cessation programs can help—smoking worsens retinal inflammation.
-
Supplements: Ask Dr. Rhue about vitamin D (a common deficiency in South Florida’s sun-conscious population).
Pediatric Inflammatory Eye Conditions
Juvenile idiopathic arthritis (JIA) affects 1 in 1,000 children, often with silent, vision-threatening uveitis. Early detection is key:
-
Warning Signs:
-
Eye redness after outdoor sports in Tamarac parks.
-
Unexplained clumsiness (blurred vision).
-
-
Action Steps:
-
Schedule pediatric eye exams if JIA is diagnosed.
-
Our clinic partners with Joe DiMaggio Children’s Hospital for complex cases.
-
Innovations in Inflammatory Eye Disease Care
West Broward Eyecare stays ahead with cutting-edge tools:
-
AI Imaging Analysis: Detects early retinal vascular changes linked to lupus.
-
Biomarker Testing: Collaborates with labs to analyze tear fluid for cytokines (no blood draw needed).
-
Clinical Trials: Ask about enrolling in studies for next-gen biologics at our Tamarac location.
Act Now for Healthier Eyes. To book an appointment, call 954-726-0204 or book online at any time!
FAQs
-
Inflammation is your body’s natural response to injury or infection, helping it heal. However, excessive inflammation without a clear cause can lead to chronic inflammatory diseases like rheumatoid arthritis or lupus.