Diabetic Retinopathy Explained: Save Your Sight Today
Introduction
Diabetic retinopathy silently threatens the vision of nearly 10 million Americans with diabetes, yet early detection and proactive management can preserve your sight for life.
Key Takeaways
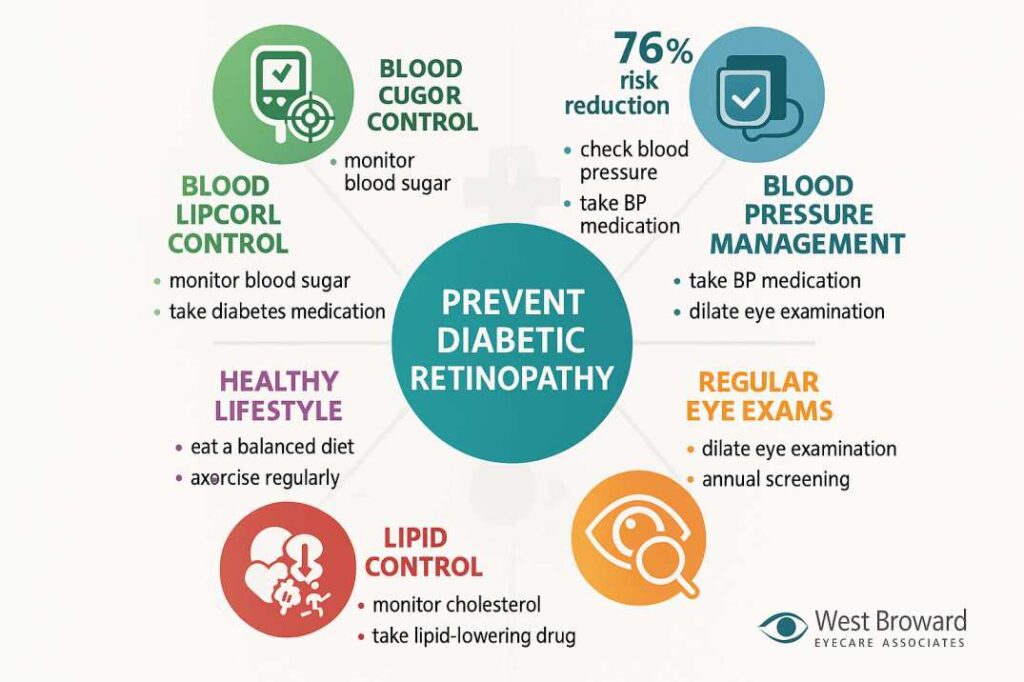
- Diabetic retinopathy is preventable: Managing blood sugar, blood pressure, and cholesterol levels can reduce your risk by up to 76%
- Early detection saves vision: Regular comprehensive eye exams can detect changes before symptoms appear.
- Treatment is more effective than ever: New therapies, including anti-VEGF injections and continuous delivery systems, offer better outcomes.
- You control the outcome: Lifestyle modifications and consistent diabetes management are your strongest defense.
- No symptoms doesn’t mean no problem: Nearly 30% of people with diabetes have some degree of retinopathy without knowing it.
Understanding Diabetic Retinopathy: The Silent Vision Thief
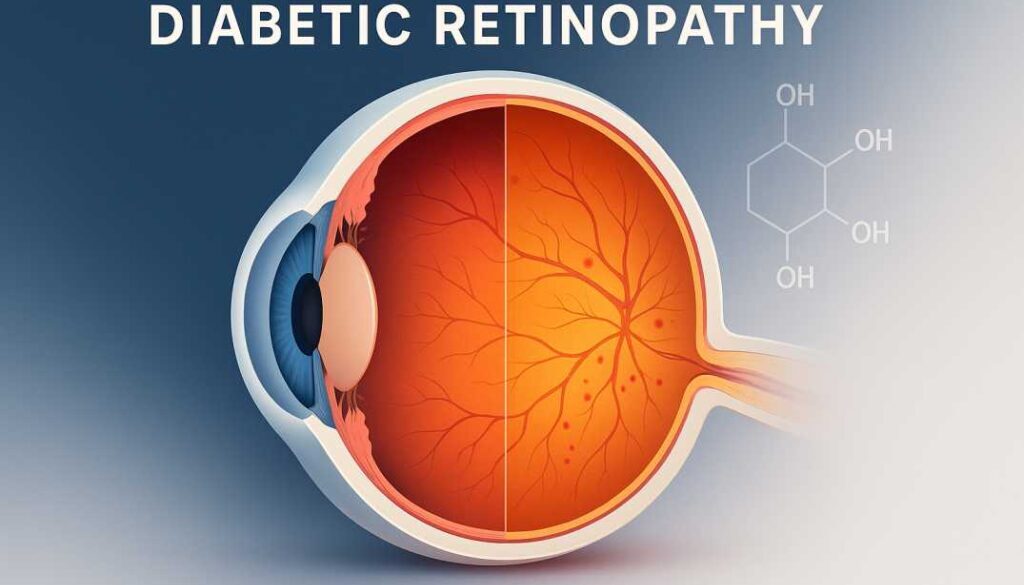
Diabetic retinopathy represents one of the most serious complications of diabetes mellitus, affecting blood vessels in the retina—the light-sensitive tissue at the back of your eye that transmits visual information to your brain. This condition develops when chronically elevated blood glucose levels damage the delicate capillaries supplying your retina, leading to vision impairment and potentially blindness if left untreated.
What Makes Diabetic Retinopathy So Dangerous?
The insidious nature of diabetic retinopathy lies in its asymptomatic early stages. Most people experience no warning signs until significant, often irreversible damage has occurred. This silent progression makes regular screening absolutely critical for anyone living with diabetes.
According to the American Diabetes Association’s 2025 Standards of Care, diabetic retinopathy affects approximately 28.5% of adults aged 40 and older with diabetes. More alarmingly, projections indicate that global cases will surge to 160 million by 2045, driven by rising diabetes prevalence worldwide.
The Impact on Your Daily Life
Beyond clinical statistics, diabetic retinopathy profoundly impacts quality of life. The condition can:
- Compromising your ability to drive safely, especially at night
- Make reading and detailed work increasingly difficult
- Affect your independence and daily activities
- Create anxiety about future vision loss
- Impact employment opportunities and career advancement
- Strain family relationships as loved ones become caregivers
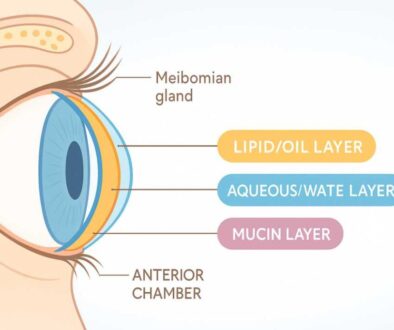
How Diabetes Damages Your Vision: The Biological Cascade
Understanding the pathophysiology of diabetic retinopathy empowers you to take targeted preventive action. The disease process unfolds through multiple interconnected mechanisms.
The Vascular Damage Pathway
When blood glucose remains elevated over time, several harmful processes damage retinal blood vessels:
1. Pericyte Loss and Capillary Weakening
- High glucose causes pericytes (cells that support blood vessel walls) to die.
- Without pericyte support, capillary walls bulge outward, forming microaneurysms.
- These are the earliest detectable signs of diabetic retinopathy.
2. Vascular Permeability and Leakage
- Damaged vessel walls become permeable, leaking fluid and blood
- Lipids and proteins accumulate in the retina as “hard exudates”
- Fluid buildup in the macula causes diabetic macular edema (DME)
3. Ischemia and Hypoxia
- Progressive vessel damage reduces blood flow to the retinal tissue
- Areas of the retina become oxygen-deprived (ischemic)
- The retina responds by releasing vascular endothelial growth factor (VEGF)
4. Pathological Neovascularization
- VEGF triggers the growth of new, abnormal blood vessels
- These vessels are fragile, bleeding easily into the vitreous gel
- Scar tissue formation can pull on the retina, causing detachment
Beyond Blood Vessels: The Neurodegeneration Factor
Recent research reveals that diabetic retinopathy isn’t purely a vascular disease. Neurodegeneration—damage to retinal nerve cells—begins early in the disease process, even before vascular changes become apparent.
Key neurological changes include:
- Ganglion cell death: Nerve cells that transmit visual signals deteriorate
- Glial cell dysfunction: Support cells fail to protect neurons properly
- Synaptic alterations: Communication between retinal nerve cells breaks down
- Neurotransmitter imbalances: Chemical signaling becomes disrupted
This neurovascular paradigm shift has important implications for early intervention strategies, suggesting that neuroprotective therapies may complement traditional vascular-focused treatments.
The Inflammatory Connection
Chronic inflammation plays a central role in diabetic retinopathy progression. Elevated blood glucose triggers an inflammatory cascade involving:
- Increased cytokine production (IL-6, IL-8, TNF-α)
- Activation of inflammatory pathways (NF-κB signaling)
- Leukocyte adhesion to blood vessel walls
- Breakdown of the blood-retinal barrier
Understanding these inflammatory mechanisms has led to the development of anti-inflammatory treatment approaches, including corticosteroid implants for diabetic macular edema.
Stages of Diabetic Retinopathy: Knowing What to Expect
Diabetic retinopathy progresses through distinct stages, each requiring different management approaches. Early recognition of these stages guides treatment decisions and helps prevent progression.
Stage 1: No Apparent Retinopathy
At this initial stage, your retina appears normal on examination despite having diabetes. However, subclinical changes may already be occurring at the cellular level.
What’s happening:
- No visible vascular damage yet
- Possible early neurodegeneration (not visible on standard exams)
- Blood glucose levels may still be damaging retinal cells
Management focus:
- Optimize diabetes control (target HbA1c 6-7%)
- Annual comprehensive dilated eye exams
- Establish baseline retinal imaging
Stage 2: Mild Nonproliferative Diabetic Retinopathy (NPDR)
The earliest clinically detectable stage, characterized by microaneurysms—tiny bulges in retinal blood vessels.
Clinical signs:
- Microaneurysms are visible on examination
- Possible small retinal hemorrhages
- No vision symptoms are typically present
Management approach:
- Continue aggressive diabetes management
- Increase screening frequency to every 6-12 months
- Monitor blood pressure and cholesterol
- Consider more frequent monitoring during pregnancy
Stage 3: Moderate Nonproliferative Diabetic Retinopathy
Vascular damage becomes more extensive, with increased risk of progression.
Clinical features:
- More numerous microaneurysms and hemorrhages
- Retinal blood vessel blockage begins
- Cotton-wool spots (nerve fiber layer infarcts) may appear
- Hard exudates (lipid deposits) are visible
- Vision may remain normal or show mild changes
Treatment considerations:
- Very close monitoring every 3-6 months
- Optimization of all systemic risk factors
- Patient education about symptoms requiring urgent attention
- Prepare for potential treatment needs
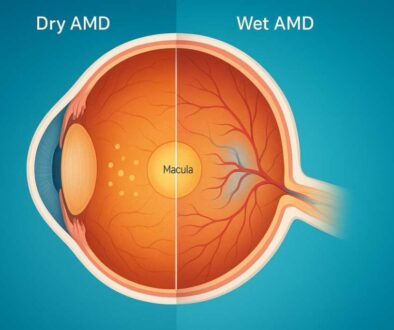
Diabetic Macular Edema: A Complication Across All Stages
Diabetic macular edema (DME) represents a separate but related complication that can occur at any stage of diabetic retinopathy.
What is DME? Fluid accumulation in the macula—the central retina responsible for sharp, detailed vision—causes swelling and vision impairment.
Impact on vision:
- Blurred central vision
- Difficulty reading or recognizing faces
- Colors appear washed out or faded
- Distorted vision (straight lines appear wavy)
Treatment options:
- Anti-VEGF intravitreal injections (first-line therapy)
- Corticosteroid implants for persistent cases
- Focal laser photocoagulation
- Combination approaches for refractory DME
Recognizing Diabetic Retinopathy Symptoms: When to Seek Care
The challenge with diabetic retinopathy symptoms is their delayed appearance. By the time symptoms develop, significant retinal damage has often occurred. However, recognizing these warning signs enables timely intervention.
Early-Stage Symptoms (Often Absent)
In mild to moderate nonproliferative diabetic retinopathy, most people experience:
- No symptoms whatsoever
- Completely normal vision
- No pain or discomfort
This asymptomatic period underscores why regular screening is non-negotiable for anyone with diabetes.
Intermediate Symptoms
As the disease progresses, you might notice:
Visual Changes:
- Fluctuating vision that varies throughout the day
- Difficulty focusing, especially when reading
- Increased difficulty with night vision
- Need for frequent prescription changes
Macular Edema Symptoms:
- Blurred or wavy central vision
- Difficulty reading fine print
- Colappearring less vivid
- Straight appearing curved (metamorphopsia)
Advanced-Stage Warning Signs
These symptoms indicate significant disease progression requiring urgent evaluation:
Floaters and Flashes:
- Sudden appearance of numerous dark spots or strings
- Cobweb-like shadows floating in your vision
- Brief flashes of light in peripheral vision
- Large dark area or “curtain” blocking vision
Severe Vision Changes:
- Sudden, dramatic vision loss
- Complete loss of vision in one eye
- Dense cloud or veil obscuring vision
- Severe distortion of images
Other Concerning Symptoms:
- Persistent eye pain or pressure
- Redness that doesn’t resolve
- Double vision
- Difficulty seeing at night
Emergency Symptoms Requiring Immediate Care
Contact an eye care professional or visit an emergency department immediately if you experience:
- Sudden complete vision loss
- Sudden onset of many floaters
- Curtain or shadow across your visual field
- Severe eye pain with vision changes
- Sudden dramatic increase in floaters following eye trauma
Risk Factors: Who’s Most Vulnerable to Diabetic Retinopathy?
While anyone with diabetes can develop retinopathy, certain risk factors significantly increase your vulnerability. Understanding these helps you take targeted preventive action.
Non-Modifiable Risk Factors
Duration of Diabetes
- Risk increases progressively with diabetes duration
- Nearly all type 1 diabetics develop some degree of retinopathy within 20 years
- Two-thirds of type 2 diabetics are affected over time
- Each additional year with diabetes incrementally raises the risk
Type of Diabetes
- Type 1 diabetes: Higher overall prevalence of retinopathy
- Type 2 diabetes: May have retinopathy at diagnosis (indicating undiagnosed diabetes existed for years)
- Latent autoimmune diabetes (LADA): Similar risks to type 1
Genetics and Ethnicity
- Family history of diabetic retinopathy increases risk
- African Americans, Hispanics, and Native Americans face higher rates
- Certain genetic polymorphisms affect susceptibility
- Asian populations are seeing how the increasing prevalence
Age
- Older age at diabetes diagnosis correlates with faster progression
- Puberty accelerates retinopathy in type 1 diabetes
- Age-related factors compound diabetic eye disease risk
Modifiable Risk Factors: Your Areas of Control
Glycemic Control (Most Critical)
- Every 1% reduction in HbA1c decreases retinopathy risk by approximately 35%
- Target HbA1c: 6-7% (individualized based on other factors)
- Rapid glucose normalization can temporarily worsen retinopathy (early worsening phenomenon)
- Glycemic variability (fluctuations) may independently increase risk
Blood Pressure Management
- Hypertension doubles retinopathy risk
- Target blood pressure: <140/90 mmHg (general); <130/80 mmHg (some guidelines)
- Both systolic and diastolic elevation contribute to risk
- Intensive BP control reduces retinopathy incidence by 34%
Lipid Abnormalities
- Elevated LDL cholesterol correlates with hard exudate formation
- High triglycerides des associated with retinopathy severity
- Dyslipidemia contributes to macular edema
- Lipid-lowering therapy (fenofibrate) shows promise in reducing progression
Kidney Disease
- Diabetic nephropathy and retinopathy share common microvascular The presence of one strongly predicts the other.
- Proteinuria (protein in urine) correlates with retinopathy severity
- Aggressive nephropathy treatment may be the right fit eyes
Lifestyle and Behavioral Factors
Smoking
- Increases diabetic retinopathy risk by 1.5 to 2-fold
- Promotes vascular damage through multiple mechanisms
- Cessation improves overall diabetes outcomes
- Secondhand smoke exposure is also harmful
ObesityA
- BMI above 30 kg/m² increases the risk
- Visceral adiposis is particularly problematic
- Weight loss improves diabetes control and reduces complications
- Bariatric surgery shows promise for diabetes remission
Physical InactivA sedentary
- Tary lifestyle worsens diabetes control
- Regular exercise improves insulin sensitivity
- Moderate activity reduces retinopathy progression
- Combine aerobic and resistance training for the best results
Alcohol Consumption
- Moderate consumption: Uncertain effects
- Heavy drinking: Worsens diabetes control and increases risk
- Alcohol can cause dangerous glucose fluctuations
- Abstinence or moderation is recommended
Pregnancy and Hormonal Factors
Pregnancy
- Existing retinopathy can rapidly worsen during pregnancy
- Riis’s highest in the first and the postpartum period, also carries a continued risk
- Requires specialized monitoring (exams every trimester)
- Blood sugar targets are stricter during pregnancy
Gestational Diabetes
- Women with gestational diabetes don’t need routine retinal screening during pregnancy.
- However, increased future diabetes risk warrants vigilance
- Screen for diabetes postpartum and regularly thereafter
Medical and Treatment Factors
GLP-1 Receptor Agonists
- Medications like semaglutide (Ozempic, Wegovy) and liraglutide
- Rapid glucose reduction may cause early retinopathy worsening
- Long-term effects are unclear but concerning in some studies
- Requires an ophthalmology assessment before initiating
- More frequent monitoring during treatment initiation
Cataract Surgery
- Can accelerate diabetic retinopathy progression postoperatively
- Screen carefully before surgery
- Optimize diabetes control perioperatively
- Monitor closely after surgery
Anemia
- Low hemoglobin levels correlate with increased retinopathy
- May reflect poor nutrition or kidney disease
- Correction of anemia mia beneficial
Prevention Strategies: Your Action Plan for Protecting Vision
The most empowering truth about diabetic retinopathy is that it’s largely preventable through systematic risk factor management and early detection. Here’s your comprehensive prevention roadmap.
Primary Prevention: Stopping Retinopathy Before It Starts
1. Achieve and Maintain Optimal Glycemic Control
The landmark Diabetes Control and Complications Trial (DCCT) and UK Prospective Diabetes Study (UKPDS) definitively proved that intensive glucose management dramatically reduces retinopathy risk.
Practical glucose targets:
- HbA1c: 6-7% (individualized based on age, comorbidities, hypoglycemia risk)
- Fasting glucose: 80-130 mg/dL
- Post-meal glucose: <180 mg/dL at 1-2 hours
- Time in range: 70% or more (continuous glucose monitoring metric)
Strategies for better control:
- Work with a certified diabetes educator
- Use continuous glucose monitoring to identify patterns
- Adjust medications as needed with your healthcare team
- Count carbohydrates accurately
- Time insulin doses appropriately with meals
- Recognize and treat hypoglycemia promptly
Important caveat: When rapidly improving poor glucose control, do so gradually under medical supervision. Rapid normalization can cause temporary retinopathy worsening (early worsening phenomenon), though long-term benefits far outweigh this risk.
2. Control Blood Pressure Aggressively
Target goals:
- General target: <140/90 mmHg
- Stricter target for some: <130/80 mmHg
- Individualize based on age and comorbidities
Blood pressure management strategies:
- Take antihypertensive medications as prescribed
- Reduce sodium intake to <2,300 mg daily (ideally <1,500 mg)
- Maintain a healthy weight
- Exercise regularly (150 minutes weekly of moderate activity)
- Limit alcohol consumption
- Manage stress through relaxation techniques
- Monitor blood pressure at home regularly
3. Optimize Lipid Levels
Target lipid values:
- LDL cholesterol: <100 mg/dL (ideally <70 mg/dL with cardiovascular disease)
- HDL cholesterol: >40 mg/dL (men), >50 mg/dL (women)
- Triglycerides: <150 mg/dL
- Non-HDL cholesterol: <130 mg/dL
Lipid management approaches:
- Statin therapy for most adults with diabetes over age 40
- Fenofibrate may provide additional retinal protection beyond cardiovascular benefits
- Dietary modifications (reduce saturated fats, increase omega-3 fatty acids)
- Weight management
- Regular physical activity
4. Adopt a Vision-Protective Diet
Certain dietary patterns and nutrients show promise for reducing diabetic retinopathy risk:
The Mediterranean Diet
- High in vegetables, fruits, whole grains, legumes
- Emphasizes olive oilomega-3-rich rich fish
- Limited red meat and processed foods
- Associated with lower retinopathy risk
Key protective nutrients:
- Omega-3 fatty acids (EPA, DHA): Found in fatty fish, walnuts, flaxseed
- Lutein and zeaxanthin: Dark leafy greens, egg yolks
- Vitamin D: Fatty fish, fortified dairy, sunlight exposure
- Antioxidants: Colorful fruits and vegetables
- Magnesium: Nuts, seeds, whole grains, leafy greens
Foods to emphasize:
- Fatty fish (salmon, mackerel, sardines): 2-3 times weekly
- Dark leafy greens (spinach, kale, collards): Daily
- Colorful vegetables: Variety throughout the week
- Berries: Rich in anthocyanins
- Nuts and seeds: Small amounts daily
- Whole grains over refined carbohydrates
Foods to limit:
- Refined sugars and sweets
- Processed foods with trans fats
- Sugar-sweetened beverages
- Excessive red meat
- High-sodium foods
5. Engage in Regular Physical Activity
Exercise improves diabetes control through multiple mechanisms and may directly protect against retinopathy.
Exercise recommendations:
- Aerobic activity: 150 minutes weekly of moderate intensity (brisk walking, swimming, cycling)
- Resistance training: 2-3 sessions weekly of all major muscle groups
- Flexibility exercises: Stretching, yoga, tai chi
- Daily movement: Break up sitting time every 30 minutes
Exercise safety with diabetic retinopathy:
- Mild to moderate NPDR: No restrictions on activity
- Severe NPDR: Avoid activities that increase eye pressure (heavy weightlifting, high-impact sports, straining)
- Proliferative retinopathy: Avoid vigorous exercise until treated and stabilized
- Always check blood glucose before, during (if prolonged), and after exercise
6. Eliminate Tobacco Use
If you smoke or use tobacco products, quitting is one of the most impactful steps you can take.
Smoking cessation resources:
- Prescription medications (varenicline, bupropion)
- Nicotine replacement therapy (patches, gum, lozenges)
- Behavioral counseling and support groups
- Text messaging and app-based programs
- Quitlines: 1-800-QUIT-NOW (1-800-784-8669)
Benefits of quitting:
- Improved diabetes control within weeks
- Reduced cardiovascular disease risk
- Lower risk of all diabetes complications
- Better response to diabetes medications
Secondary Prevention: Catching Problems Early
1. Comprehensive Dilated Eye Examinations
Regular screening detects retinopathy in its earliest, most treatable stages.
Screening schedule:
Type 1 Diabetes:
- First exam: Within 5 years of diagnosis
- Frequency: Annually if no retinopathy
- More frequent if retinopais thy present
Type 2 Diabetes:
- First exam: At time of diagnosis (may have had undiagnosed diabetes for years)
- Frequency: Annually if no retinopathy
- Every 6-12 months with mild NPDR
- Every 3-6 months with moderate NPDR
- Every 2-4 months with severe NPDR
Pregnancy:
- Exams before pregnancy or in the first trimester
- Each trimester is based on findings
- 1 year postpartum follow-up
- Gestational diabetes only: No retinal screening needed during pregnancy
What happens during a comprehensive exam:
- Visual acuity testing
- Pupil dilation with drops (causes temporary blurred near vision)
- Slit lamp examination of eye structures
- Dilated fundus examination of the retina
- Optional: Retinal photography for documentation
- Optional: Optical coherence tomography (OCT) for macular assessment
2. Advanced Screening Technologies
Modern screening methods enhance early detection:
Retinal Photography with Remote Reading
- Wide-field fundus cameras capture detailed retinal images
- Images sent to ophthalmologists for remote interpretation
- Increases screening access in underserved areas
- Comparable accuracy to in-person examination
Artificial Intelligence Screening
- FDA-approved AI algorithms analyze retinal images
- Detects referable diabetic retinopathy with high accuracy
- Provides immediate results
- Expands screening capacity
Optical Coherence Tomography (OCT)
- Cross-sectional imaging of retinal layers
- Detects macular edema with precision
- Monitors treatment response
- Identifies subtle structural changes
Fluorescein Angiography
- Dye injection highlights blood vessel abnormalities
- Identifies areas of leakage and non-perfusion
- Guides treatment decisions
- Reserved for more advanced cases or unclear diagnoses
3. Home Monitoring and Self-Examination
While not a substitute for professional screening, self-monitoring helps you detect concerning changes early.
Amsler grid testing:
- Simple at-home test for macular problems
- Grid of horizontal and vertical lines
- Check each eye separately
- Look for wavy lines, missing areas, or distortion
- Test weekly if you have diabetic retinopathy
Visual symptom awareness:
- Note any new floaters or flashes
- Monitor for vision fluctuations
- Document changes in your vision diary
- Report any concerns promptly to your eye doctor
4. Patient Education and Empowerment
Understanding your condition empowers you to take control:
- Learn about diabetic retinopathy stages and progression
- Understand how your blood sugar, blood pressure, and cholesterol affect your eyes
- The new warning signs require urgent evaluation
- Communicate openly with your healthcare team
- Ask questions about treatment options and decisions
- Connect with support groups and patient communities
Tertiary Prevention: Managing Established Retinopathy
If you’ve already developed diabetic retinopathy, these strategies prevent progression and preserve remaining vision.
1. Continued Risk Factor Optimization
Systemic control remains crucial even after retinopathy develops:
- Maintain target HbA1c, blood pressure, and lipids
- Don’t assume “it’s too late” – prevention still works at every stage
- Work closely with both the endocrinologist and the ophthalmologist
2. Close Monitoring
Increased surveillance frequency catches progression early:
- Follow your ophthalmologist’s recommended schedule
- Don’t skip appointments even if your vision feels fine
- Bring a list of all medications and recent HbA1c results
3. Prompt Treatment
When your ophthalmologist recommends treatment:
- Understand the rationale and expected benefits
- Discuss risks and alternatives
- Follow through with scheduled treatments
- Report side effects or concerns
4. Lifestyle Modifications
Even with established retinopathy, lifestyle changes help:
- Continue a healthy diet and exercise
- Manage stress through relaxation techniques
- Get adequate sleep (7-9 hours nightly)
- Stay socially connected and engaged
Current Treatment Options: What’s Available in 2025
Diabetic retinopathy treatment has advanced dramatically, offering better visual outcomes and more convenient administration than ever before.
Anti-VEGF Therapy: The Cornerstone of Modern Treatment
Vascular endothelial growth factor (VEGF) inhibitors have revolutionized diabetic retinopathy treatment.
How Anti-VEGF Works:
- Blocks VEGF, a protein that stimulates abnormal blood vessel growth and leakage
- Reduces vascular permeability and macular edema
- Causes regression of neovascularization
- Improves vision in many cases (not just stabilization)
Available Anti-VEGF Medications:
1. Aflibercept (Eylea)
- FDA-approved for diabetic retinopathy and DME
- Blocks multiple VEGF isoforms plus placental growth factor
- Typically given every 4-8 weeks initially
- High-dose aflibercept (Eylea HD) allows less frequent dosing in some patients.
2. Ranibizumab (Lucentis)
- Extensively studied in diabetic eye disease
- DRCR.net trials demonstrate efficacy
- Usually administered monthly or as-needed
- Generic version becoming available, reducing cost
3. Bevacizumab (Avastin)
- Used off-label (not FDA-approved for eye disease)
- Similar efficacy to ranibizumab and aflibercept
- Significantly less expensive
- Wide adoption despite off-label status
4. Brolucizumab (Beovu)
- Newest anti-VEGF agent
- Small molecule size may enhance retinal penetration
- An extended dosing interval is possible
- Rare but serious inflammatory complications require careful monitoring
5. Faricimab (VabyA bispecific
- Specific antibody blocking both VEGF and angiopoietin-2
- Approved for DME and proliferative diabetic retinopathy
- May allow longer intervals between injections
- Promising durability data
Treatment Protocol:
- Intravitreal injection (into the eye) in an office setting
- Quick procedure with topical anesthesia
- Loading phase: Often 3-6 monthly injections initially
- Maintenance: Extended intervals based on response
- Ongoing monitoring and retreatment as needed
What to Expect:
- Slight pressure sensation during injection
- Mild discomfort or irritation for 24 hours
- Floaters may appear (usually from medication or air bubbles)
- Vision improves gradually over weeks to months
- Multiple injectables are typically required
Results:
- Diabetic macular edema: 40-50% gain ≥15 letters (3 lines) of vision
- Proliferative retinopathy: High rates of regression without laser
- Earlier treatment → better outcomes
- Some patients achieve complete resolution
Continuous Delivery Systems: The Future Is Here
Susvimo (Ranibizumab Port Delivery System)
A breakthrough FDA-approved in 2025 for diabetic retinopathy, Susvimo offers continuous anti-VEGF delivery.
How It Works:
- Surgically implanted refillable ocular implant
- Continuously releases ranibizumab into the eye
- Refilled every 9 months in the office procedure
- Eliminate the need for frequent injections
Benefits:
- Maintains vision with just 1-2 refills annually versus 8-12+ injections
- More predictable drug levels
- Reduced treatment burden on patients
- Fewer office visits
Considerations:
- Requires initial surgical implantation
- Higher initial risk of endophthalmitis (eye infection) compared to injections
- Best for patients requiring ongoing anti-VEGF therapy
- May not be suitable for all patients
Laser Photocoagulation: Still Valuable
While anti-VEGF has become the first-line therapy, laser treatment remains important.
Panretinal Photocoagulation (PRP)
Indications:
- Proliferative diabetic retinopathy (high-risk PDR)
- Alternatively, when anti-VEGF is contraindicated or unavailable
- Adjunct to anti-VEGF in some cases
How it works:
- Applies 1,200-2,000 laser burns to the peripheral retina
- Reduces the oxygen demand of the retina
- Decreases VEGF production
- Causes abnormal vessels to regress
Procedure:
- Usually 1-2 sessions
- Topical or local anesthesia
- 20-40 minute procedure
- May cause temporary discomfort
Side effects:
- Peripheral vision loss (expected)
- Night vision difficulties
- Reduced accommodation (focusing ability)
- Rarely, worsening of macular edema
Focal/Grid Laser for DME
Purpose:
- Treats diabetic macular edema
- Seals leaking microaneurysms
- Now generally reserved for cases not responsive to anti-VEGF
Technique:
- Precise laser application to leaking areas
- Grid pattern for diffuse edema
- Usually, an outpatient procedure
Corticosteroid Treatments
Steroid medications reduce inflammation and vascular leakage in diabetic macular edema.
Available Options:
1. Dexamethasone Implant (Ozurdex)
- A biodegradable implant is injected into the eye
- Slowly release steroids over 3-6 months
- Typically used when anti-VEGF therapy is insufficient
- May be first-line in pseudophakic eyes (after cataract surgery)
2. Fluocinolone Implant (Iluvien)
- Non-biodegradable implant
- Releaseroid for up to 3 years
- Reserved for chronic, persistent DME
- Requires fewer retreatments
Considerations:
- Increased risk of cataract formation
- Possible intraocular pressure elevation requiring management
- May accelerate cataract in phakic patients (with natural lens)
- Regular IOP monitoring is essential
Vitrectomy Surgery
For advanced complications, vitreoretinal surgery becomes necessary.
Indications:
- Non-clearing vitreous hemorrhage (blood in the eye)
- Tractional retinal detachment
- Severe proliferative retinopathy
- Combined traction and rhegmatogenous detachment
Procedure:
- Perform the d in the operating room
- Removes vitreous gel from the eye
- Peels scar tissue (membranes)
- May include endolaser treatment
- Gas or oil tamponade if detachments are present
Recovery:
- Vision improves gradually, weeks to months
- Positioning requirements if gas/oil is used
- Cataract develops monocular vision within 1-2 years
- Generally good outcomes if performed timely
Emerging and Investigational Treatments
The future of diabetic retinopathy treatment looks promising:
1. Gene Therapy
- Delivers VEGF-blocking genes directly to retinal cells
- Single treatment potentially provides years of effect
- Currently in clinical trials
2. Stem Cell Therapy
- Adipose-derived and bone marrow stem cells show promise
- May regenerate damaged retinal tissue
- Reduce inflammation and neovascularization
- Still largely experimental
3. Nanotechnology
- Nanoparticle drug delivery systems
- Targeted retinal delivery with sustained release
- Reduced systemic side effects
- Early research stages
4. PPARα Modulators
- Fenofibrate and pemafibrate
- Reduce lipids and inflammation
- May slow retinopathy progression
- Oral medication (not injection)
- Clinical trials ongoing
5. Neuroprotective Agents
- Target retinal neurodegeneration
- Aim to prevent early damage before vascular changes
- Multiple candidates in development
Special Populations: Tailored Approaches
Different groups require specific considerations in diabetic retinopathy management.
Pregnancy and Diabetic Retinopathy
Pregnancy presents unique challenges and risks for diabetic retinopathy.
Why Pregnancy Increases Risk:
- Hormonal changes affect retinal vasculature
- Rapid glucose normalization attempted
- Hemodynamic changes increase vascular stress
- Increased VEGF levels
Management During Pregnancy:
Pre-conception:
- Comprehensive eye exam before attempting pregnancy
- Optimize diabetes control gradually (avoid rapid changes)
- Treat significant retinopathy before conception if possible
During PregnaExamine
- Examine each trimester
- More frequent if retinopathy is present
- Close coordination between the obstetrician, endocrinologist, and ophthalmologist
- Laser treatment is safe during pregnancy if needed
- Anti-VEGF: VEGF is generally avoided (theoretical fetal risks)
Postpartum:
- Retinopathy may continue progressing postpartum
- Exam at 3-6 months postpartum
- Resume normal screening schedule
- Is VEGF safe while breastfeeding (minimal systemic absorption)
Pediatric Patients
Children and adolescents with type 1 diabetes require special consideration.
Screening Recommendations:
- First exam: 5 years after diabetes diagnosis or age 11 (whichever comes later)
- Annual exams thereafter if no retinopathy
- Puberty accelerates progression – increase vigilance
Unique Considerations:
- Balancing tight control with hypoglycemia risk
- Psychosocial factors affecting adherence
- Long-term exposure risk (decades with diabetes)
- Technology adoption (pumps, CGM) may help
Elderly Patients
Older adults face additional challenges in diabetic retinopathy management.
Complicating Factors:
- Multiple comorbidities
- Polypharmacy
- Cognitive decline affecting self-management
- Transportation barriers to appointments
- Medicare coverage considerations
Adapted Management:
- Individualized HbA1c targets (less stringent in frail elderly)
- Simplified medication regimens
- Involve the caregiver in the care plan
- Telemedicine options when appropriate
- Home-based monitoring tools
Patients with Kidney Disease
Diabetic nephropathy and retinopathy commonly coexist.
Why They’re Connected:
- Shared microvascular pathology
- Common risk: The presence of one predicts the other
Management Implications:
- Proteinuria predicts retinopathy severity
- More aggressive ophthalmology monitoring if nephropathy is present
- Some medications require dose adjustment with reduced kidney function
- Coordinate care between the nephrologist and the ophthalmologist
Living with Diabetic Retinopathy: Practical Guidance
If you’ve been diagnosed with diabetic retinopathy, these strategies help you maintain the best possible quality of life.
Coping with Vision Changes
- Magnifying glasses and handheld magnifiers
- Large-print books and electronics
- Text-to-speech software
- High-contrast settings on devices
- Task lighting for reading and detailed work
Home Modifications:
- Improve lighting throughout the house
- Reduce glare with window treatments
- Mark the stairs and edges with contrasting colors
- Organize belongings in consistent locations
- Use voice-activated devices
Mobility Support:
- White cane training for those with severe vision loss
- Guide dogs for the blind
- Orientation and mobility specialists
- GPS and navigation apps with voice guidance
Driving with Diabetic Retinopathy
Driving represents a major independence concern.
Safety Considerations:
- Vision requirements vary by state (typically 20/40 or better)
- Regular vision tests if retinopsent
- Avoid night driving if impaired
- Limit challenging driving situations
- Consider alternatives (rideshare, public transit) as needed
When to Stop Driving:
- Vision below state minimum requirements
- Significant peripheral vision loss
- Difficulty judging distances
- Recent retinopathy progression
- Recommendation from an ophthalmologist
Emotional and Psychological Support
Vision loss and fear of blindness significantly impact mental health.
Common Emotional Responses:
- Anxiety about future vision loss
- Depression from lifestyle limitations
- Frustration with treatment burden
- Grief over lost independence
- Isolation from social withdrawal
Support Resources:
- Mental health counseling
- Support groups for vision loss
- Diabetes support communities
- Family counseling
- Online forums and communities
Organizations Providing Support:
- American Foundation for the Blind
- National Federation of the Blind
- VisionAware
- American Diabetes Association support programs
- Local low vision rehabilitation services
Employment and Daily Activities
Many people with diabetic retinopathy continue working and leading active lives.
Workplace Accommodations:
- Screen reading software
- Large monitors and magnification
- Voice recognition software
- Adjustable lighting
- Flexible schedules for medical appointments
Daily Life Adaptations:
- Smartphone accessibility features
- Talking watches and appliances
- Large-button phones
- Labeled organization systems
- Audiobooks and podcasts
Financial Considerations
Diabetic retinopathy treatment and management involve significant costs.
Insurance Coverage:
- Medicare Part B covers diabetic eye exams and treatment
- Most private insurance covers medically necessary treatment
- Some plans require prior authorization for anti-VEGF
- Understanding coverage before treatment reduces surprises
Cost-Saving Strategies:
- Patient assistance programs from drug manufacturers
- Generic medications, when available (bevacizumab off-label)
- Non-profit organizations offering financial help
- Flexible spending accounts (FSA) for out-of-pocket costs
- Discuss costs openly with your healthcare team
Building Your Healthcare Team
Optimal diabetic retinopathy management requires coordination among specialists.
Your Core Team:
Ophthalmologist/Retina Specialist:
- Diagnoses and treats eye complications
- Performs procedures (injections, laser, surgery)
- The Ines monitoring schedule
Endocrinologist/Diabetologist:
- Optimizes diabetes management
- Adjusts medications
- Manages other diabetes complications
Primary Care Physician:
- Coordinates overall care
- Manages blood pressure, lipids
- Addresses other health concerns
Certified Diabetes Educator:
- Teaches self-management skills
- Helps with nutrition and lifestyle
- Provides ongoing support
Optometrist:
- May perform screening exams
- Refer to an ophthalmologist when needed
- Provides glasses/contact lenses
Additional Team Members:
- Nephrologist (if kidney disease ease present)
- Cardiologist (if heart disease ease present)
- Mental health professional
- Social worker
- Low vision specialist
Latest Trends and Innovations in Diabetic Retinopathy Care
The field of diabetic retinopathy is rapidly evolving with exciting developments.
Artificial Intelligence in Screening
AI-powered diagnostic systems are transforming screening accessibility:
Current Applications:
- FDA-approved algorithms detect referable diabetic retinopathy
- Instant results during screening visits
- High sensitivity (87%) and specificity (90%)
- Expanding screening capacity in primary care settings
Future Directions:
- AI prediction of disease progression risk
- Automated treatment response monitoring
- Integration with electronic health records
- Deep learning severity grading
Telemedicine and Remote Monitoring
Teleophthalmology increases screening reach:
Virtual Screening Programs:
- Retinal imaging at convenient locations
- Remote reading by ophthalmologists
- Triage of high-risk patients for in-person care
- Particularly valuable in rural/underserved areas
Home Monitoring Technologies:
- Portable retinal cameras for home use (investigational)
- AI-assisted apps detecting vision changes
- Remote vision testing applications
- Smartphone-based screening tools
Novel Drug Delivery Systems
Beyond Susvimo, additional continuous delivery metare hods in development:
Hydrogel Implants:
- Biodegradable polymers releasing anti-VEGF
- Less invasive than current implants
- Varied release kineare tics possible
Microneedle Patches:
- Painless drug delivery to the eye
- Sustained release formulations
- Potential for self-administration
Suprachoroidal Injection:
- Alternative to intravitreal injection
- Drug delivery to the hind retina
- May have different pharmacokinetics
Combination Therapies
Multi-targeted approaches show promise:
Anti-VEGF Plus Anti-Inflammatory:
- Combining anti-VEGF with steroid implants
- May enhance efficacy in resistant cases
- Addressing multiple disease mechanisms
Dual Pathway Inhibition:
- Faricimab blocks both VEGF and Ang-2
- Others in development targeting additional pathways
- More comprehensive vascular stabilization
Personalized Medicine
Tailoring treatment to individual patient characteristics:
Genetic Profiling:
- Identifying genetic risk factors
- Predicting treatment response
- Customizing prevention strategies
Biomarker-Guided Treatment:
- Inflammatory markers
- Circulating VEGF levels
- Proteomic signatures
- Individualized treatment intensity
Creating Your Personalized Diabetic Retinopathy Prevention Plan
Translating knowledge into action requires a personalized approach. Use this framework to develop your plan.
Step 1: Assess Your Current Risk
Complete this risk assessment:
- ☐ How long have you had diabetes? ______ years
- ☐ What is your most recent HbA1c? _____%
- ☐ What is your blood pressure? /
- ☐ Do you have other diabetes complications (kidney disease, neuropathy)?
- ☐ Do you smoke or use tobacco?
- ☐ When was your last comprehensive eye exam? ______
- ☐ Do you have any diabetic retinopathy now? If yes, what stage? ______
- ☐ Is diabetes well-controlled or requiring adjustment?
Your risk level:
- High risk: Diabetes >15 years, HbA1c >8%, existing retinopathy, poor BP control
- Moderate risk: Diabetes 5-15 years, HbA1c 7-8%, some risk factors present
- Lower risk: Diabetes <5 years, HbA1c <7%, well-controlled, no complications
Step 2: Set SMART Goals
Create Specific, Measurable, Achievable, Relevant, Time-bound goals.
Examples:
- “Lower my HbA1c from 8.2% to 7.5% within 3 months”
- “Scheda ule comprehensive eye exam by [specific date]”
- “Reduce blood pressure to <140/90 through medication and 30-minute daily walks”
- “Lose 10 pounds in 3 months through portion control and exercise”
- “Quit smoking by [date] using nicotine replacement and support group”
Step 3: Build Your Action Plan
Daily Actions:
- Check blood glucose as prescribed
- Take medications as scheduled
- Eat meals aligned with the meal plan
- Exercise for ______ minutes
- Document value the s in the health app/journal
Weekly Actions:
- Grocery shop using a healthy food list
- Meal prep for the upcoming week
- Review glucose patterns
- Check blood pressure _____ times
- Engage in a stress-reduction activity
Monthly Actions:
- Attend medical appointments
- Review HbA1c, BP, lipid trends
- Assess progress toward goals
- Adjust plan as needed
Annual Actions:
- Comprehensive dilated eye exam
- Complete blood work panel
- A1c check (unless done more frequently)
- Urine microalbumin screening
- Foot examination
Step 4: Overcome Common Barriers
Identify your obstacles and solutions:
“I forgot to take my medication. ions”
- Set phone alarms
- Use a pill organizer
- Link to daily routine (e.g., brushing teeth)
- Ask about long-acting formulations
“Healthy food is expensive.”
- Buy seasonal produce
- Use frozen vegetables (equally nutritious)
- Shop sales and use coupons
- Cook at home instead of eating out
- Buy store brands
“I don’t have time to exercise.”
- Break into 10-minute segments throughout the day
- Walk during lunch break
- Exercise while watching TV
- The stairs instead of the elevator
- Park farther away from destinations
“I can’t afford eye exams.”
- Check insurance benefits (often covered)
- Community health centers offer a sliding scale
- Lions Club provides free screening in some areas
- Discuss payment plans with the provider
- Don’t skimp p – cost of blindness, which far exceeds prevention
Step 5: Track Your Progress
Monitoring keeps you accountable and motivated.
Metrics to Track:
- Blood glucose readings
- HbA1c results
- Blood pressure
- Weight
- Medication adherence
- Exercise frequency and duration
- Nutrition goals
- Eye exam attendance
Tracking Tools:
- Health apps (MyFitnessPal, MySugr, Glucose Buddy)
- Continuous glucose monitors
- Blood pressure monitors
- Smart scales
- Paper journals
- Spreadsheets
Step 6: Celebrate Successes
Acknowledge achievements, both large and small:
- HbA1c reaching target
- Weight loss milestones
- Completing an eye exam
- Consecutive days of medication adherence
- Exercise streaks
- Blood pressure improvements
Reward yourself with non-food treats:
- New workout clothes
- Book or magazine
- Massage or spa treatment
- Movie or concert
- Hobby supplies
Taking Action Today: Your Next Steps
You now have comprehensive knowledge about diabetic retinopathy prevention and management. The final critical component is taking action.
Immediate Actions (This Week)
- Schedule your comprehensive eye exam if you haven’t had one in the past year (or per your recommended schedule)
- Check your most recent HbA1c, blood pressure, and lipid levels – know your numbers. numbers
- Review your current medications and ensure you’re taking them as prescribed. ribed
- Take one photo of yourself today to document your commitment to eye health
- Tell one trusted person about your commitment to preventing diabetic retinopathy
Short-Term Actions (This Month)
- Meet with your healthcare team to discuss your diabetes management plan
- Make one dietary improvement (reduce sugar, add vegetables, control portions)
- Start or increase physical activity with a goal of 150 minutes weekly
- Create a medication schedule and adherence system
- Research support resources in your community
Long-Term Commitment (Ongoing)
- Attend all scheduled appointments with your healthcare team
- Monitor your diabetes control through regular testing and adjustments
- Practice healthy lifestyle habits consistently
- Stay informed about new developments in diabetic retinopathy care
- Support others with diabetes in your community
Key Research Sources and Citations
This article is built upon the latest peer-reviewed research, clinical guidelines, and authoritative medical sources from 2024-2025. Below are the primary scientific sources that informed this comprehensive guide:
Primary Research Articles
1. American Diabetes Association Standards of Care in Diabetes—2025
- Citation: American Diabetes Association Professional Practice Committee. “Retinopathy, Neuropathy, and Foot Care: Standards of Care in Diabetes—2025.” Diabetes Care 48, Supplement 1 (January 2025): S252–S265.
- Link: https://diabetesjournals.org/care/article/48/Supplement_1/S252/157552/12-Retinopathy-Neuropathy-and-Foot-Care-Standards
- Key Contributions: This source provided the 2025 clinical practice recommendations for diabetic retinopathy screening schedules, treatment protocols, and evidence-based prevention strategies. The guidelines establish that intensive diabetes management with near-normoglycemia prevents and delays diabetic retinopathy onset and progression, with specific HbA1c targets of 6-7% for most patients.
2. FDA Approval of Susvimo for Diabetic Retinopathy (Roche/Genentech, May 2025)
- Citation: Roche. “FDA Approves Susvimo® (ranibizumab injection) for Diabetic Retinopathy.” Press Release, May 22, 2025.
- Link: https://www.roche.com/media/releases/med-cor-2025-05-22
- Key Contributions: This breakthrough announcement detailed the first FDA-approved continuous delivery treatment for diabetic retinopathy. The Pavilion study (Phase III trial) demonstrated that Susvimo maintains vision with only one refill every nine months, dramatically reducing the treatment burden on patients. The study showed that approximately 10 million Americans are affected by diabetic retinopathy, and this innovation offers predictable, sustained VEGF inhibition without frequent injections.
3. Risk Prediction Models for Diabetic Retinopathy: A Systematic Review (2025)
- Citation: Huang, H., Wu, Y., Ye, H., Li, J., Chen, L., and Huang, X. “Risk Prediction Models for Diabetic Retinopathy: A Systematic Review.” Frontiers in Endocrinology 16 (2025): 1556049.
- Link: https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1556049/full
- Key Contributions: This comprehensive systematic review analyzed multiple diabetic retinopathy prediction models, enabling precision medicine approaches for identifying high-risk patients. The research emphasized that duration of diabetes, chronic hyperglycemia, nephropathy, hypertension, and dyslipidemia are the primary risk factors associated with retinopathy development and progression.
Conclusion: Your Vision Is Worth Protecting
Diabetic retinopathy stands as one of diabetes’s most feared complications, yet it’s also one of the most preventable. The research is clear and the message is hopeful: with proper diabetes management, regular screening, and timely treatment when needed, you can preserve your vision throughout your life with diabetes.
The key differentiator between those who maintain healthy vision and those who lose sight isn’t the diagnosis of diabetes itself – it’s the daily choices made in response to that diagnosis. Every blood glucose check, every healthy meal, every dose of medication, and every eye exam represents an investment in your future vision.
At West Broward Eyecare Associates, we see your world through your eyes. We understand that preserving your sight means protecting your independence, your livelihood, your ability to see your grandchildren’s faces, and your capacity to pursue the activities you love. Our commitment extends beyond clinical expertise to partnership in your long-term eye health journey.
Remember: Diabetic retinopathy doesn’t have to steal your sight. With knowledge, action, and support, Caninnta can have ain clear vision for years to come. The power to protect your eyes rests largely in your hands – and we’re here to guide you every step of the way.
Your vision is precious. Your future is clear. Take action today.
This article was created to provide comprehensive, evidence-based information about diabetic retinopathy. It is not a substitute for professional medical advice. If you have diabetes, schedule a comprehensive eye exam with West Broward Eyecare Associates or your local ophthalmologist today.
FAQs
-
Diabetic retinopathy damages small blood vessels in the retina, causing vision blurriness, swelling, or even blindness if untreated.