Eye Flashes and Floaters: When to Worry vs When to Wait
Quick Answer: Most eye floaters and flashes are harmless age-related changes, but sudden increases, vision loss, or new symptoms warrant immediate evaluation to rule out retinal tears or detachment.
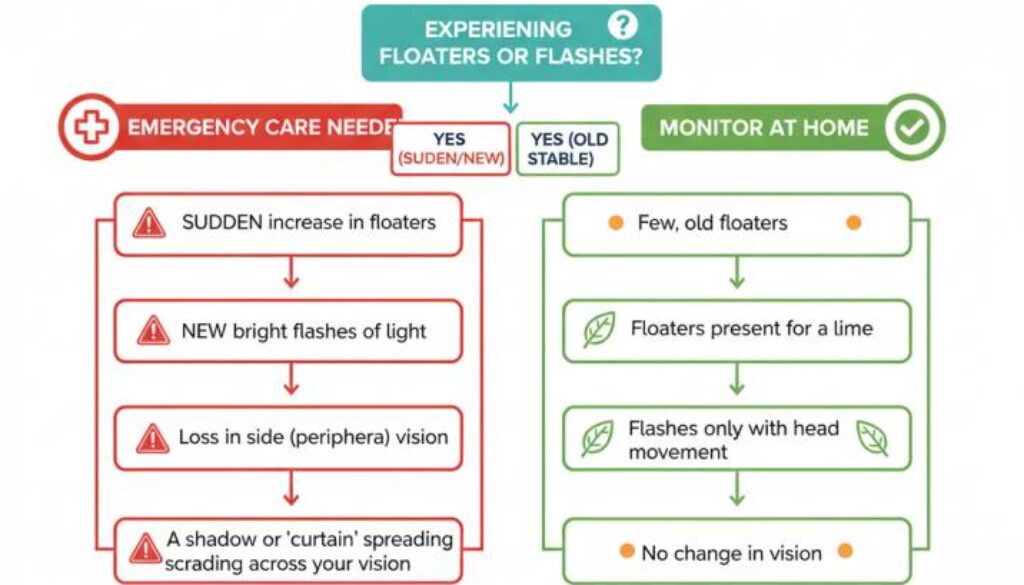
When to Wait vs. When to Worry
✅ When to Wait and Monitor:
- Occasional eye floaters you’ve had for years
- Mild flashes during head movement
- Gradual changes are developing over months
- Floaters that appear in bright light only
🚨 When to Seek Emergency Care:
- Sudden shower of new floaters
- Frequent flashes lasting hours
- Curtain-like shadows in vision
- Any combination of these symptoms
Understanding Eye Flashes and Floaters
What Are Eye Floaters?
Eye floaters appear as small, dark shapes drifting across your vision—they might look like spots, threads, squiggly lines, or cobwebs. While they seem to float in front of your eyes, floaters actually exist inside your eye, casting shadows on your retina.
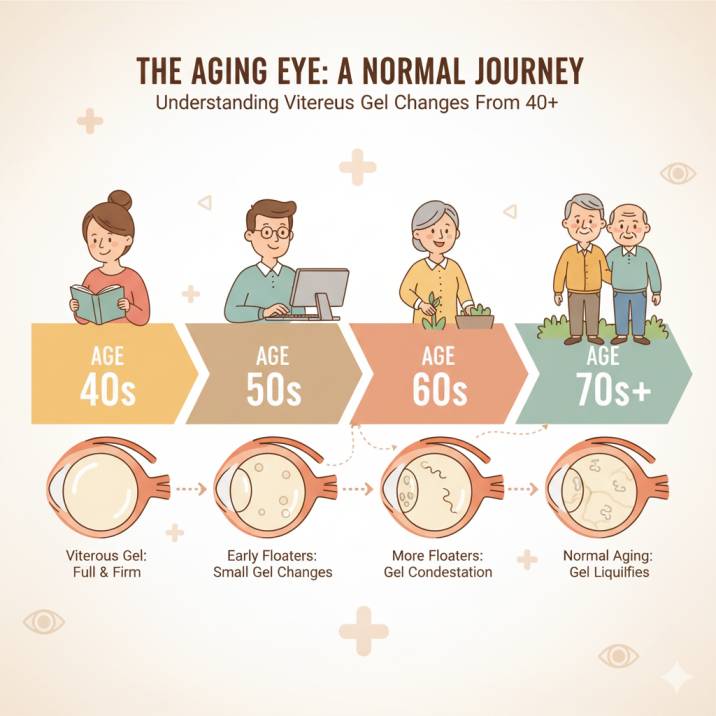
The primary cause of most floaters is the vitreous humor, a clear, gel-like substance that fills about 80% of your eye and helps maintain its round shape. As you age, this gel gradually changes from a firm, jelly-like consistency to a more liquid state. During this process, tiny clumps of collagen and protein fibers form within the vitreous, creating the shadows you see as floaters.
Understanding Eye Flashes (Photopsias)
Eye flashes, medically called photopsias, appear as brief bursts of light, sparks, or streaks in your vision. Unlike floaters that drift and linger, flashes are typically quick and occur at the edges of your visual field.
Flashes happen when the vitreous gel tugs on your retina as it shrinks and contracts with age. Since the retina doesn’t have pain receptors, this mechanical stimulation manifests as flashes of light—essentially your retina’s way of responding to physical stress.
Posterior Vitreous Detachment (PVD) Explained
Posterior vitreous detachment is one of the most common causes of new floaters and flashes in people over 50. This natural aging process occurs when the vitreous gel separates from the retina’s surface.
During PVD, you might experience:
- A sudden increase in floaters
- Flashes of light, especially in peripheral vision
- A large, ring-shaped floater (called a Weiss ring)
- Cobweb-like shapes in your vision
The process typically takes weeks to months to complete, and symptoms usually diminish once the vitreous fully detaches.
Emergency Warning Signs: When Every Minute Counts
While most floaters and flashes are benign, certain warning signs demand immediate medical attention. These symptoms could indicate serious conditions like retinal tears or detachment, which require prompt treatment to prevent vision loss.
🚨 Seek Emergency Eye Care If You Experience:
Sudden Onset of Multiple Floaters
If you wake up one morning seeing dozens of new floaters—particularly if they look like “pepper sprinkled in your vision”—this could signal a retinal tear with bleeding.
Persistent or Frequent Flashes
Flashes that occur repeatedly over hours or days, especially if they’re visible with your eyes closed, may indicate ongoing retinal traction.
Curtain or Shadow in Peripheral Vision
Any dark area or shadow that seems to block part of your side vision could indicate retinal detachment—a true eye emergency.
Combination of Symptoms
The simultaneous appearance of new floaters, flashes, and vision changes is particularly concerning and requires immediate evaluation.
Vision Loss or Blurriness
Any decrease in central or peripheral vision accompanying floaters or flashes suggests possible retinal complications.
The 24-48 Hour Rule
Recent research shows that retinal tears detected within 24-48 hours of symptom onset have significantly better treatment outcomes. Don’t wait to “see if it gets better”—early intervention can preserve your vision.
Normal Age-Related Changes: What to Expect
Understanding normal age-related eye changes can help you distinguish between typical aging and concerning symptoms.
The Aging Eye Timeline:
Ages 40-50: Early Changes Begin
The vitreous starts to become less gel-like, and some people notice their first floaters. This is normal.
Ages 50-65: PVD Becomes Common
About 66% of people between the ages of 66-86 experience posterior vitreous detachment, with over 75% of those over age 65 developing the condition. Symptoms during this period are usually temporary.
Ages 65+: Adaptation Phase
Most people adapt to their floaters, and new symptoms become less frequent as the vitreous stabilizes in its detached state.
Risk Factors for Earlier Changes:
High Myopia (Nearsightedness) People with significant nearsightedness often experience floaters and PVD at younger ages due to the elongated shape of their eyes.
Previous Eye Surgery: Cataract surgery and other eye procedures can trigger earlier vitreous changes, though this doesn’t necessarily indicate complications.
Eye Traum: Previous eye injuries can disrupt normal vitreous structure, leading to earlier floater development.
Diabetes Diabetic changes can affect the vitreous, though this is typically associated with other diabetic eye complications.
Latest Research and Treatment Advances in 2025
Recent studies have provided new insights into floater management and PVD outcomes, offering hope for patients struggling with bothersome symptoms.
Current Research Findings:
Improved Risk Assessment
A 2024 prospective study of 1,010 patients with flashes and floaters found that 9.9% of those with confirmed PVD had retinal tears, emphasizing the importance of comprehensive examination for new symptoms.
Enhanced Surgical Outcomes
Recent advances in vitrectomy techniques have improved safety profiles for floater removal surgery, though it’s still reserved for severe cases that significantly impact quality of life.
New Treatment Options
Low-dose atropine drops are being investigated in clinical trials as a potential treatment for bothersome floaters, with ongoing research evaluating their effectiveness. Several treatment options are currently in development for severe cases.
Treatment Philosophy in 2025:
Modern eye care emphasizes:
- Early detection through advanced imaging
- Conservative management for benign cases
- Prompt intervention for sight-threatening conditions
- Patient education to reduce anxiety and improve quality of life
Your Action Plan: A Decision-Making Framework
Knowing how to respond to floaters and flashes can reduce anxiety and ensure you get appropriate care when needed.
The STOP Method for Symptom Assessment:
S – Sudden or Gradual? Sudden changes are more concerning than gradual ones. Mark the date when new symptoms began.
T – Type and Pattern Document what you’re seeing: Are they floaters, flashes, or both? Do they occur together or separately?
O – Other Symptoms Note any accompanying vision loss, eye pain, or other changes in your sight.
P – Previous History: Consider your personal and family eye history, age, and risk factors.
Creating Your Monitoring System:
Keep a Visual Symptom Diary
Track new symptoms, their frequency, and any triggers you notice. This information helps your eye doctor assess whether changes are concerning.
Establish a Baseline
During routine eye exams, discuss your typical floater pattern with your doctor so future changes can be properly evaluated.
Know Your Risk Factors
Understanding your personal risk profile helps both you and your doctor make informed decisions about symptom evaluation.
Prevention and Lifestyle Strategies
While you can’t prevent normal aging changes, certain lifestyle factors may help maintain overall eye health and reduce the risk of complications.
Eye Health Fundamentals:
Regular Comprehensive Eye Exams
Annual exams for people over 60, or as recommended based on your risk factors, help detect problems before symptoms appear.
Blood Sugar Management
For diabetic patients, maintaining good glucose control reduces the risk of diabetic eye complications that can accelerate vitreous changes.
Blood Pressure Control
Hypertension can affect retinal blood vessels, potentially increasing the risk of complications during PVD.
UV Protection
While not directly related to floaters, UV protection supports overall retinal health and may reduce other age-related eye conditions.
Stress and Anxiety Management:
Many people experience significant anxiety about floaters and flashes. Consider these strategies:
Education and Understanding
Learning about normal eye anatomy and aging can reduce fear about common symptoms.
Mindfulness and Adaptation Techniques
Some patients find that meditation and focusing exercises help them adapt more quickly to benign floaters.
Professional Support
For severe anxiety about eye symptoms, counseling or support groups can be beneficial.
When Professional Evaluation is Essential
Understanding when to seek professional care ensures you receive appropriate treatment while avoiding unnecessary anxiety.
Schedule Prompt Evaluation For:
New Symptom Onset
Any new floaters or flashes, regardless of severity, warrant professional assessment to establish a baseline and rule out complications.
Symptom Progression
Gradual worsening of existing symptoms over weeks or months should be evaluated to ensure no underlying pathology is developing.
Quality of Life Impact
If floaters significantly interfere with your daily activities, reading, or driving, discuss treatment options with your eye care provider.
What to Expect During Your Examination:
Comprehensive Dilated Exam
Your doctor will use special drops to widen your pupils and examine your retina thoroughly for tears, detachment, or other abnormalities.
Advanced Imaging
OCT (Optical Coherence Tomography) and other imaging technologies can detect subtle changes not visible during standard examination.
Visual Field Testing
If retinal problems are suspected, specialized testing may evaluate your peripheral vision for areas of loss.
Supporting Your Family Through Eye Health Changes
Floaters and flashes often cause anxiety not just for patients but for family members who want to help and understand what’s happening.
For Family Members:
Take Symptoms Seriously
Even if floaters seem minor, acknowledge the patient’s concerns and support appropriate medical evaluation.
Learn the Warning Signs
Understanding emergency symptoms helps family members know when to encourage immediate medical care.
Support Adaptation
Many people successfully adapt to benign floaters with time and understanding. Patience and encouragement during this process are valuable.
Creating a Supportive Environment:
Reduce Visual Stress
During the adaptation period, adjusting lighting and screen time can help minimize floater visibility.
Encourage Professional Care
Support regular eye examinations and prompt evaluation of new symptoms without creating unnecessary anxiety.
Maintain Perspective
While concerning, most floater and flash episodes resolve without complications. Balanced concern and optimism help reduce stress for everyone involved.
Key Takeaways: Your Essential Guide
✅ Most Cases Are Benign: The vast majority of floaters and flashes represent normal aging changes that don’t threaten vision.
⏰ Timing Matters: Sudden onset of symptoms requires prompt evaluation, while gradual changes can often be monitored.
🚨 Know the Warning Signs: A Shower of floaters, persistent flashes, and vision loss are red flags requiring immediate care.
🛡️ Prevention is Key: Regular eye exams and overall health management support optimal eye aging.
🧠 Adaptation is Possible: Many people successfully adjust to benign floaters and lead normal, active lives.
👩⚕️ Professional Partnership: Developing a relationship with a trusted eye care provider ensures appropriate monitoring and intervention when needed.
Additional Resources and Citations
Key Medical Sources Used in This Article:
1. Posterior Vitreous Detachment and Retinal Tear Research (2024)
- Source: Nixon, T.R.W., Davie, R.L., Snead, M.P. “Posterior vitreous detachment and retinal tear – a prospective study of community referrals”
- Link:
https://www.nature.com/articles/s41433-023-02779-3 - Key Finding: Prospective study of 1,010 patients showing a 9.9% rate of retinal tears in confirmed PVD cases, emphasizing the importance of comprehensive examination
2. Large-Scale PVD Complications Analysis (2022)
- Source: Vestrum Health Database Study – “Analysis of Posterior Vitreous Detachment and Development of Complications Using a Large Database of Retina Specialists“
- Link:
https://www.sciencedirect.com/science/article/abs/pii/S2468653022005759 - Key Finding: Study of 9,635 eyes showing a 25% complication rate with acute symptomatic PVD over 6-month follow-up, with a higher risk in men and pseudophakic eyes
3. Advanced OCT Imaging Research (2025)
- Source: “Posterior Vitreous Detachment in Healthy Versus AMD Eyes Assessed by Widefield Optical Coherence Tomography”
- Link:
https://pmc.ncbi.nlm.nih.gov/articles/PMC12154524/ - Key Finding: Recent research shows higher rates of complete PVD in AMD patients (74-75%) compared to healthy controls (55%) using advanced imaging technology
Expert Medical Guidelines Referenced:
Cleveland Clinic Eye Health Resources
https://my.clevelandclinic.org/health/diseases/14413-posterior-vitreous-detachment
Harvard Health Publishing – Eye Floaters and Flashes
https://www.health.harvard.edu/blog/what-you-can-do-about-floaters-and-flashes-in-the-eye-201306106336
American Academy of Ophthalmology Clinical Guidelines: Multiple peer-reviewed sources for emergency eye care protocols and patient education standards
Conclusion: Balancing Vigilance with Peace of Mind
Understanding flashes and floaters empowers you to make informed decisions about your eye health while reducing unnecessary anxiety about common aging changes. The key is developing the knowledge to distinguish between normal variations and symptoms requiring urgent attention.
Remember that your eyes, like the rest of your body, change with age. Most of these changes are harmless adaptations to the natural aging process. However, staying alert to warning signs and maintaining regular professional care ensures that any serious problems are caught early when treatment is most effective.
Whether you’re experiencing your first floater or learning to live with long-standing visual changes, know that modern eye care offers excellent outcomes for both benign conditions and serious complications when they’re properly identified and managed.
Your vision is precious, and taking a balanced, informed approach to floater and flash symptoms helps protect it while maintaining your quality of life and peace of mind.
About West Broward Eyecare Associates
Our experienced team provides comprehensive eye care services, including emergency eye care, retinal evaluations, and advanced diagnostic imaging. Located in Tamarac, Florida, we serve families throughout West Broward County with the latest technology and compassionate, expert care.
Emergency Eye Care: If you’re experiencing a sudden onset of floaters, flashes, or vision changes, contact our office immediately or visit our emergency eye care page.
Schedule a Consultation: Regular eye exams are essential for maintaining healthy vision. Contact us today to schedule your comprehensive eye examination.
FAQs
-
Eye floaters are small specks, dots, or cobweb-like shapes drifting across your vision, caused by vitreous gel changes as it liquefies with age. Sudden floaters may signal vitreous detachment or retinal issues requiring immediate evaluation.