Stop Vision Loss Early: Managing High Eye Pressure
High eye pressure, or ocular hypertension, occurs when intraocular pressure (IOP) exceeds the normal range of 10-21 mmHg. At West Broward Eyecare Associates, we specialize in advanced screening to detect this “silent” condition before it progresses to irreversible vision loss or glaucoma.
What is High Eye Pressure?
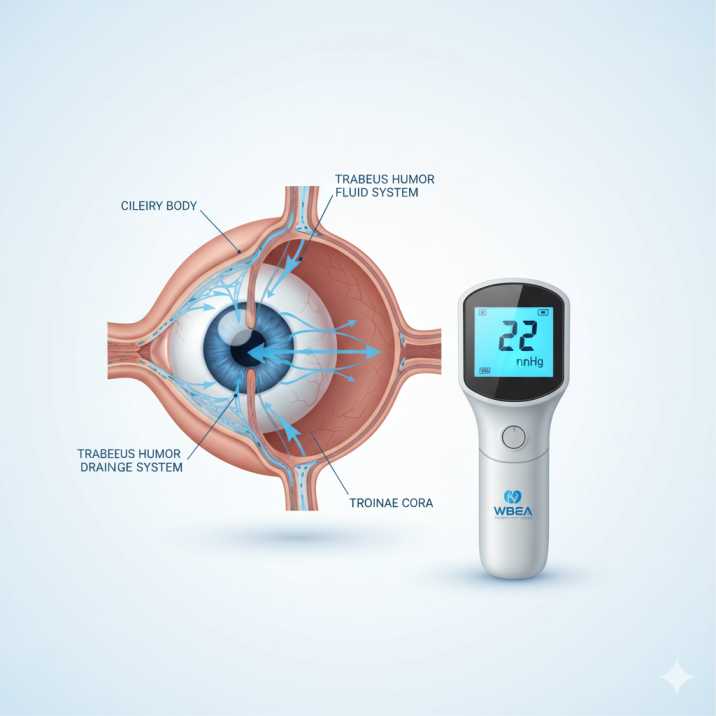
Your eyes aren’t hollow chambers—they’re filled with a clear fluid called aqueous humor that nourishes your eye tissues and maintains proper eye shape. Think of it like the water pressure in your home’s plumbing system. When this fluid doesn’t drain properly, pressure builds up inside your eye.
Normal eye pressure ranges from 10-21 millimeters of mercury (mmHg). When your intraocular pressure (IOP) consistently measures above 21 mmHg, eye care professionals classify this as high eye pressure or ocular hypertension.
How Eye Pressure Works
Your eyes constantly produce aqueous humor through a structure called the ciliary body. This fluid flows through your pupil, nourishes the front of your eye, and drains through a mesh-like system called the trabecular meshwork. When this drainage system becomes blocked or inefficient, pressure accumulates—similar to a clogged drain, causing water to back up.
The Numbers That Matter
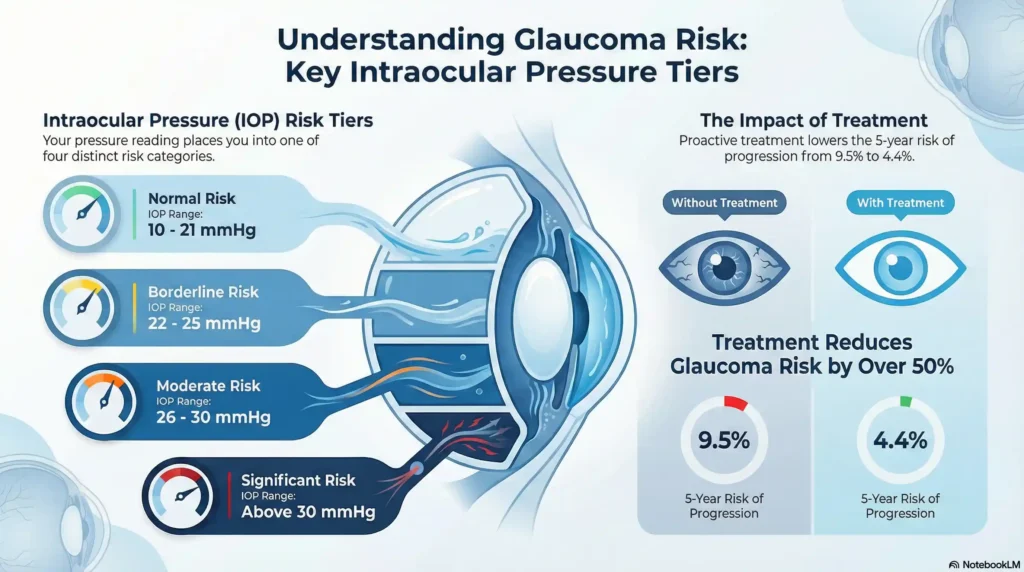
Recent studies from the Ocular Hypertension Treatment Study (OHTS) reveal critical statistics:
- Normal pressure: 10-21 mmHg
- Borderline elevation: 22-25 mmHg
- Moderate elevation: 26-30 mmHg
- Significant elevation: Above 30 mmHg
Understanding Ocular Hypertension
Ocular hypertension represents the middle ground between normal eye pressure and glaucoma. You have elevated pressure, but no detectable damage to your optic nerve or vision loss—yet. This condition affects approximately 4-10% of Americans over age 40, making it one of the most common eye-related concerns we encounter at our Tamarac practice.
Why “Silent” Conditions Are Concerning
Unlike a headache or eye pain that immediately gets your attention, ocular hypertension typically produces no symptoms. You can’t feel the elevated pressure, and your vision remains clear. This silent nature makes regular eye exams crucial, especially for our patients in the West Broward community who may have family histories of glaucoma or other risk factors.
The Progression Timeline
Research from Harvard Medical School and the National Eye Institute shows that ocular hypertension doesn’t automatically become glaucoma. In fact:
- Only 9.5% of untreated patients develop glaucoma within 5 years
- With treatment, this risk drops to approximately 4.4%
- Over 90% of people with ocular hypertension never develop vision loss
These statistics underscore why we emphasize individualized care—not everyone needs immediate treatment, but everyone needs careful monitoring.
The Silent Connection to Glaucoma Risk
Glaucoma, often called the “silent thief of sight,” damages the optic nerve gradually and irreversibly. High eye pressure isn’t the only cause of glaucoma, but it’s the most significant modifiable risk factor. Understanding this connection helps explain why we take ocular hypertension seriously.
How Pressure Damages Vision
The optic nerve contains over one million nerve fibers that carry visual information from your eye to your brain. When pressure inside your eye exceeds what these delicate fibers can withstand, they begin to die. Unlike other body tissues, optic nerve fibers can’t regenerate—making prevention crucial.
Types of Glaucoma Risk
Primary Open-Angle Glaucoma: The most common type, where the drainage angle remains open but functions poorly. Pressure builds gradually, and vision loss typically begins in your peripheral (side) vision.
Normal-Tension Glaucoma: Some people develop glaucoma even with normal eye pressure, emphasizing that pressure is just one factor in a complex disease process.
Secondary Glaucoma: Results from other eye conditions, medications (particularly steroids), or trauma that affects fluid drainage.
Recent Research Insights
A 2024 study published in the American Journal of Ophthalmology followed patients from the OHTS for over 20 years, revealing that some participants experienced rapid vision loss despite careful monitoring. This reinforces our commitment to regular follow-up appointments and personalized treatment plans for our Tamarac families.
Risk Factors You Should Know
Understanding your personal risk profile helps us develop the most appropriate monitoring and treatment strategy. Risk factors fall into two categories: those you can’t change and those you can influence.
Non-Modifiable Risk Factors
Age: Your risk increases significantly after age 40, with the highest rates occurring after age 60. For our senior patients in Tamarac’s active adult communities, this makes regular eye exams particularly important.
Family History: Having a parent or sibling with glaucoma increases your risk by 4-9 times. We often see multiple family members in our practice, which helps us track familial patterns.
Ethnicity: African Americans face a 6-8 times higher risk of developing glaucoma compared to other ethnic groups, often at younger ages and with more aggressive progression.
Corneal Thickness: Thinner corneas may indicate higher actual pressure than measurements suggest, while thicker corneas might mask true pressure levels.
Modifiable Risk Factors
High Blood Pressure: While high blood pressure can slightly increase eye pressure, very low blood pressure actually poses greater glaucoma risk by reducing blood flow to the optic nerve.
Diabetes: Diabetic patients face increased glaucoma risk through multiple mechanisms, including changes in blood vessels and fluid dynamics.
Medication Use: Long-term steroid use (eye drops, injections, or oral medications) can significantly elevate eye pressure.
Eye Trauma: Previous eye injuries can disrupt normal fluid drainage, sometimes causing pressure problems months or years later.
Symptoms and Detection
The absence of symptoms makes ocular hypertension particularly challenging for patients to self-detect. Unlike acute angle-closure glaucoma, which causes severe eye pain, nausea, and blurred vision, ocular hypertension typically produces no warning signs.
Rare Symptoms
In unusual cases, patients might experience:
- Mild eye discomfort when moving the eyes
- Slight headaches (though these are more often related to other factors)
- Very subtle halos around lights
Professional Detection Methods
During comprehensive eye exams, we use several methods to measure eye pressure accurately:
Goldmann Applanation Tonometry: The gold standard for pressure measurement, using a small probe to gently touch your eye’s surface after numbing drops.
Non-Contact Tonometry: The “air puff” test that many patients recognize, useful for screening but less precise than contact methods.
Handheld Tonometry: Devices like the Tono-Pen or iCare tonometer, particularly useful for children or patients who have difficulty with traditional methods.
Comprehensive Evaluation
Detecting ocular hypertension requires more than just pressure measurement. Our complete evaluation includes:
- Visual Field Testing: Maps your peripheral vision to detect early glaucoma changes
- Optic Nerve Assessment: Direct examination and photography to document nerve appearance
- Corneal Thickness Measurement: Ensures accurate pressure interpretation
- Angle Examination: Determines if your drainage system is structurally normal
Treatment Options and Management
Not everyone with ocular hypertension requires immediate treatment. We base treatment decisions on your individual risk profile, considering factors like pressure level, age, family history, and other risk factors.
Risk Stratification
Low Risk: Young patients with mildly elevated pressure, no family history, and normal optic nerves may only need monitoring every 6-12 months.
Moderate Risk: Patients with multiple risk factors or borderline findings might benefit from treatment or more frequent monitoring every 3-6 months.
High Risk: Older patients with significantly elevated pressure, thin corneas, or suspicious optic nerve changes typically benefit from immediate treatment.
Treatment Options
Topical Medications: Eye drops remain the first-line treatment, with several classes available:
- Prostaglandin analogs (once daily, very effective)
- Beta-blockers (twice daily, well-tolerated)
- Alpha agonists (helpful for patients with cardiovascular concerns)
- Carbonic anhydrase inhibitors (available as drops or pills)
Laser Therapy: Selective Laser Trabeculoplasty (SLT) can improve drainage without daily medications, particularly beneficial for patients who struggle with eye drop compliance.
Minimally Invasive Surgeries: For patients needing cataract surgery, newer MIGS procedures can address both conditions simultaneously.
Prevention and Lifestyle Strategies
While you can’t change genetic risk factors, several lifestyle modifications may help maintain healthy eye pressure and overall eye health.
Dietary Considerations
Research suggests certain nutrients may support eye health:
- Omega-3 fatty acids: Found in fish, flaxseeds, and walnuts
- Antioxidants: Leafy greens, berries, and colorful vegetables
- Magnesium: May help with blood flow to the optic nerve
- Limit caffeine: Large amounts can temporarily increase eye pressure
Exercise and Eye Pressure
Regular aerobic exercise can help lower eye pressure naturally. However, avoid activities that involve:
- Extended head-down positions (like certain yoga poses)
- Excessive straining or breath-holding
- High-impact activities if you have other eye conditions
Stress Management
Chronic stress may contribute to elevated eye pressure through various mechanisms. Consider:
- Regular meditation or relaxation techniques
- Adequate sleep (7-8 hours nightly)
- Managing work and family stress through healthy coping strategies
Eye Protection
Protect your eyes from trauma that could disrupt normal drainage:
- Wear safety glasses during sports and home improvement projects
- Use appropriate eye protection for work activities
- Be cautious with contact sports if you have elevated pressure
When to See Your Eye Doctor
Understanding when to seek professional care can make the difference between preserving your vision and experiencing irreversible loss.
Emergency Situations
Seek immediate medical attention for:
- Suddenly, severe eye pain
- Rapid vision loss
- Nausea and vomiting with eye pain
- Seeing halos around lights with pain
- Red eyes with severe pain
These symptoms might indicate acute angle-closure glaucoma, a medical emergency requiring immediate treatment.
Routine Screening Guidelines
Ages 18-39: Eye exams every 2-4 years unless you have risk factors.
Ages 40-54: Every 1-2 years.
Ages 55-64: Every 1-2 years,
Age 65+: Annually
Special Circumstances Requiring More Frequent Monitoring
- Family history of glaucoma: Annual exams starting at age 35
- African American heritage: Annual exams starting at age 35
- Diabetes or high blood pressure: Follow your eye doctor’s recommendations
- Previous eye trauma: Regular monitoring as advised
- Steroid medication use: More frequent pressure checks
Latest Research and Treatment Advances
The field of glaucoma and ocular hypertension treatment continues to evolve rapidly, with exciting developments offering hope for better outcomes.
2024-2025 Research Highlights
OHTS Long-Term Follow-Up: Recent 20-year data from the Ocular Hypertension Treatment Study provide unprecedented insights into long-term outcomes, helping us better predict which patients need treatment.
Genetic Research: Scientists are identifying genetic markers that may predict glaucoma risk more accurately, potentially allowing earlier intervention.
Artificial Intelligence: New AI systems can analyze optic nerve photographs and visual field tests with remarkable accuracy, potentially catching changes earlier than traditional methods.
Emerging Treatment Technologies
Direct Selective Laser Trabeculoplasty (DSLT): This revolutionary technique delivers laser treatment without requiring traditional gonioscopy, making the procedure faster and more comfortable.
Biocompatible Implants: New drainage devices made from advanced materials show promise for patients who need surgical intervention.
Neuroprotection Research: Scientists are investigating ways to protect optic nerve cells from damage, potentially preventing vision loss even when pressure remains elevated.
Pipeline Medications
Multi-Target Therapies: New drugs that work through multiple mechanisms simultaneously, potentially providing better pressure control with fewer side effects.
Extended-Release Formulations: Medications that last weeks or months, eliminating the burden of daily eye drops.
Why Choose West Broward Eyecare Associates for Ocular Hypertension Management
At West Broward Eyecare Associates, our comprehensive approach to ocular hypertension management reflects the latest evidence-based practices. Located in Tamarac and serving Parkland, Coconut Creek, Coral Springs, and surrounding communities, our practice consistently ranks #1-2 for eye care searches in our region—a testament to our commitment to exceptional patient care.
Advanced Technology for Early Detection
Our state-of-the-art facility features cutting-edge diagnostic equipment, including the Optomap® for dilation-free retina exams, allowing us to detect ocular hypertension and early glaucoma changes without the discomfort of traditional dilation. This technology is particularly valuable for our busy West Broward families who need efficient, thorough eye care.
Specialized Glaucoma Care in Tamarac
As glaucoma specialists serving the diverse communities of Broward County, we understand that early detection of ocular hypertension is crucial for our patients, particularly given the higher prevalence of glaucoma in African American populations. Our comprehensive eye exams include precise pressure measurements, optic nerve assessment, and corneal thickness evaluation—all essential components identified by the landmark Ocular Hypertension Treatment Study.
Personalized Treatment Plans
Whether you’re a young professional in Coral Springs with mildly elevated pressure or a senior in Tamarac with multiple risk factors, we develop individualized monitoring and treatment strategies. Our approach considers the latest research showing that not all patients with ocular hypertension require immediate treatment, but all benefit from careful, expert monitoring.
Community-Focused Care Statistics
- Serving 6 major communities: Tamarac, Parkland, Coconut Creek, Coral Springs, Plantation, and Sunrise
- #1-2 ranking for critical eye care searches in our region
- Specialized care for pediatric through senior populations
- Emergency eye care services for urgent ocular hypertension concerns
Contact Information:
- Location: 7822 N University Dr, Tamarac, FL 33321
- Phone: (954) 726-0204
- Email: info@wbeca.com
- Hours: Monday-Thursday 9:00 AM–5:00 PM, Friday 9:00 AM–4:00 PM
Essential Resources and Research Citations
The following three authoritative sources provide the foundation for evidence-based ocular hypertension management and represent the most current research in the field:
1. American Academy of Ophthalmology – Ocular Hypertension Guidelines
Resource Link: https://www.aao.org/eye-health/diseases/what-is-ocular-hypertension
The American Academy of Ophthalmology provides comprehensive clinical guidelines for diagnosing and managing ocular hypertension, defining it as elevated intraocular pressure without optic nerve damage or vision loss. This resource offers the latest preferred practice patterns used by eye care professionals nationwide, including specific protocols for patient monitoring, treatment decisions, and follow-up care. The AAO guidelines form the foundation for clinical decision-making at practices like West Broward Eyecare Associates, ensuring patients receive care aligned with national standards.
[Schedule Your Comprehensive Eye Pressure Exam in Tamarac]
2. National Eye Institute – Ocular Hypertension Treatment Study (OHTS)
Resource Link: https://www.nei.nih.gov (Search: Ocular Hypertension Treatment Study)
The landmark OHTS, sponsored by the National Eye Institute, represents the most comprehensive study of ocular hypertension treatment, following 1,636 patients for over 20 years to determine optimal management strategies. This groundbreaking research demonstrated that pressure-lowering treatment reduces glaucoma development by approximately 50% in high-risk patients. The study’s findings directly influence treatment protocols used throughout West Broward, helping eye care professionals determine which patients benefit most from immediate treatment versus careful observation.
3. JAMA Ophthalmology – Recent Ocular Hypertension Research (2024-2025)
Resource Link: https://jamanetwork.com/journals/jamaophthalmology
Recent publications in JAMA Ophthalmology include breakthrough studies on quality of life impacts and long-term outcomes in ocular hypertension patients, providing new insights into patient care and treatment decisions. The journal’s 2024-2025 publications feature updated analyses from the OHTS follow-up studies, genetic research for glaucoma risk prediction, and innovations in laser treatments. These findings are particularly relevant for Tamarac-area residents, as they inform modern treatment approaches, including minimally invasive procedures and personalized risk assessment tools now available at comprehensive eye care centers.
Conclusion:
High eye pressure affects millions silently, but early detection prevents up to 50% of glaucoma cases. At West Broward Eyecare Associates, our advanced Optomap® technology and expert care have helped countless Tamarac-area families protect their vision through personalized ocular hypertension management.
Don’t wait for symptoms that may never come—ocular hypertension is detected only through professional eye exams. Your vision is irreplaceable, and with today’s treatments, preventable vision loss should never occur.
Take Control of Your Eye Health Today
- Same-day appointments available
- Advanced dilation-free screening
- Serving Tamarac, Coral Springs & Parkland
- Most insurance plans are accepted
Schedule your comprehensive eye exam now—because when it comes to your eyesight, early detection saves sight.
FAQs
-
High eye pressure means increased fluid pressure inside your eye without optic nerve damage, known as ocular hypertension. It requires monitoring to prevent glaucoma risk.