Eye Emergency? Symptoms & When to Seek Immediate Care | Tamarac, FL
Sudden vision loss, physical trauma, or chemical exposure to the eye are medical emergencies that require immediate intervention to prevent permanent blindness. If you are experiencing a “curtain” over your vision, new flashes of light, or severe pain accompanied by nausea, you must seek emergency care or a same-day eye exam immediately.
Understanding Eye Emergencies
Eye emergencies can occur suddenly and may result from a variety of serious causes. Prompt evaluation is crucial to prevent vision loss. Below, we outline the symptoms and their potential causes.
Emergency Eye Problems
If, at any point, your vision goes completely black (in one eye or both) you need to see your eye doctor immediately or go straight to the emergency room. DO NOT WAIT. This could be due to a variety of causes, of which many are serious and possibly life threatening.
- Retinal detachment: may see flashes or floaters, may see curtain of black/lost vision coming over the vision.
- Impending stroke: sudden vision loss (which may return to normal) could mean a blockage in the blood flow to your eye and brain. Go to the ER immediately.
Flashes or floaters
This can be a sign that the retina is being disturbed and could mean a retinal detachment is happening. While occasional floaters and flashes are common and often harmless, certain situations require immediate medical attention.

When Flashes and Floaters are NOT Serious
- Common Floaters: If you’ve had floaters for years and they haven’t changed or increased, they’re likely a normal part of aging or the result of changes in the vitreous (the gel inside the eye).
- Occasional Flashes: Flashes of light that occur sporadically and are mild may be due to migraines or natural changes in the vitreous, especially as you age.
- Slow Onset: If floaters or flashes develop slowly over time without any other symptoms, they’re often less concerning.
When Are Flashes and Floaters Serious?
- Sudden Increase: A sudden increase in the number of floaters, especially if they look like a “shower” of specks or spots.
- Flashes with a Curtain of Darkness: If you notice flashes of light followed by a dark curtain or shadow across your vision, it could signal a retinal detachment.
📞 Need Immediate Triage? Call (954) 726-0204 for a Same-Day Emergency Exam.
- Persistent Flashes: Continuous or frequent flashes of light, especially if they’re new, can indicate the retina is being disturbed.
- Accompanying Vision Loss: If flashes or floaters are paired with partial or total loss of vision, it may point to a serious condition, like a retinal tear or detachment.
- Stroke Warning Signs: While flashes alone are not typically a sign of a stroke, if they are accompanied by sudden vision loss, confusion, slurred speech, or weakness on one side of your body, seek emergency care immediately.
Sudden decrease in vision (blurry)
If there is any sudden change to your vision that is significant, make an appointment to see your eye doctor the same day. Some causes for sudden blurry vision may be a bleed inside the eye, fluid in the retina, swelling of the optic nerve, or inflammation inside the eye.
Severe pain
Any significant pain in the eye or behind the eye should indicate you need to see your eye doctor immediately. Some causes may be spike in intraocular pressure, corneal abrasion, fluid or pressure behind the eye
*Any of these symptoms require immediate attention or an emergency room visit.
Urgent Eye Problems
- Redness – could be due to infection, inflammation, foreign body, dry eyes, subconjunctival bleed, allergies
- Mild-Moderate Pain – could be due to inflammation, abrasion, stye, pressure behind the eye
- Mild-moderate Irritation – could be due to dryness, foreign body in the eye, inflammation
- Slightly blurry vision – if vision slowly or suddenly decreases slightly, this could be due to mild fluid in the retina, corneal edema, or dryness
- You got something in your eye – whether it be an eyelash, dirt, shampoo, or a chemical the best thing to do is flush your eye with artificial tears or water and call the office. Usually these can be treated at your eye doctor, but if after hours or on the weekend, an emergency visit may be required.
*Urgent symptoms may or may not require an urgent visit to the eye doctor. It is best to call the office and discuss your symptoms to determine the best course of action.
Preventing Vision Loss: Why Acting Quickly Matters
Delaying medical care for eye emergencies can lead to permanent vision loss. If you are unsure about the severity of your symptoms, it is better to err on the side of caution and seek evaluation promptly.

First Aid for Common Eye Emergencies
Act Fast—These Steps Can Save Vision Before Reaching a Doctor in Tamarac
-
Chemical Exposure (cleaning products, solvents):
Immediately flush the eye with lukewarm water for 15+ minutes. Tilt your head sideways to avoid contaminating the other eye. Call Tamarac urgent eye care or go to the nearest ER (like Broward Health Coral Springs) if burning persists. -
Foreign Objects (dust, metal, eyelashes):
Do not rub—blink repeatedly to let tears flush it out. If stuck, use sterile saline or artificial tears. For embedded objects (e.g., metal shavings), cover the eye with a paper cup and head to a Tamarac eye emergency clinic. -
Sudden Pain or Redness:
Apply a cool compress (no pressure) and avoid OTC redness drops. Could indicate a corneal abrasion or infection—schedule a same-day exam with a Tamarac or Coral Springs optometrist. -
Blunt Trauma (sports injury, accident):
Gently ice the surrounding area (not the eyeball) to reduce swelling. Vision changes like double images? Seek immediate care—retinal detachment risks are higher in high-impact injuries.
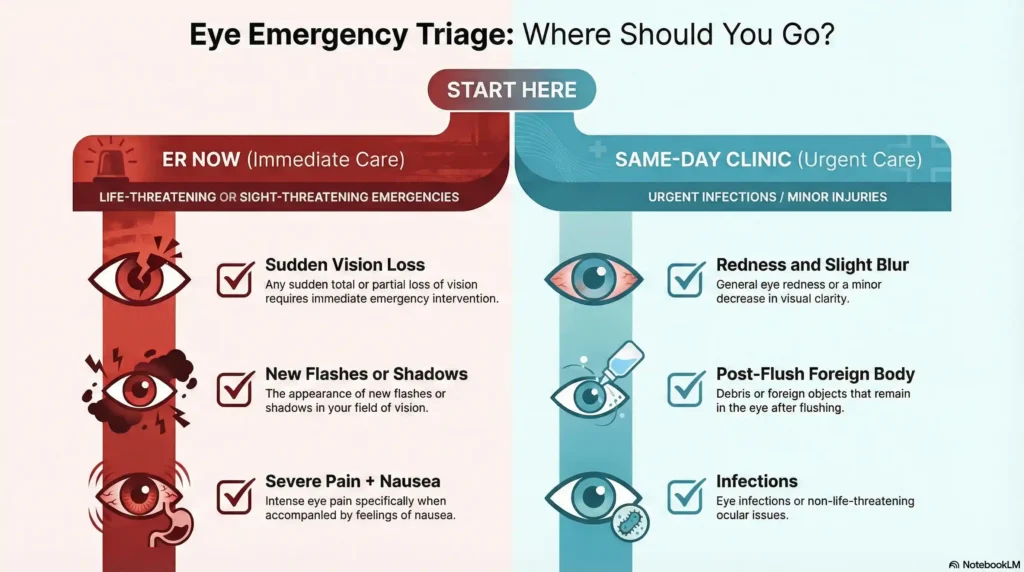
ER vs. Eye Doctor: Where to Go for Emergency Symptoms
Go to the ER Now (Broward Health, Holy Cross):
-
Vision loss lasting >5 minutes (stroke warning)
-
Knife/metal penetrating the eye
-
Chemical burns from alkalis (e.g., drain cleaners)
-
Severe pain + vomiting (acute glaucoma)
Visit a Tamarac Eye Clinic Same-Day:
-
Retinal detachment signs (shadowy curtain, new floaters)
-
Sudden blurriness without pain (possible macular issue)
-
Mild-moderate redness/pain (infections, uveitis)
-
Persistent foreign object (after flushing attempts)
Not Sure?
Call West Broward Eyecare Associates(954) 726-0204—we’ll triage your symptoms and direct you to the right.
Long-Term Recovery After an Eye Emergency
Post-emergency care is critical to avoid setbacks:
-
After Retinal Surgery (detachment repair):
Avoid heavy lifting, bending, or air travel for 2–4 weeks. Attend all follow-ups at your Tamarac retina specialist to monitor healing. -
Chemical Burn Recovery:
Use preservative-free artificial tears and steroid drops (if prescribed). Watch for cloudiness or renewed pain—signs of corneal damage needing re-evaluation. -
Post-Trauma Care (scratches, hemorrhages):
Wear sunglasses outdoors and skip contacts until cleared. Tamarac’s bright sunlight can worsen light sensitivity.
FAQs
-
Sudden vision loss, severe pain, flashes of light, or a dark curtain appearing over your vision are key signs of an emergency.
AUTHOR


