Keratoconus Guide 2026: Symptoms, Causes & Treatment
Keratoconus is a progressive eye disorder where the cornea thins and bulges into a cone-like shape, affecting approximately 1 in 345 people as of 2025. At West Broward Eyecare Associates, we specialize in advanced diagnostic technology and modern treatments like Corneal Collagen Cross-Linking (CXL) and Scleral Lenses to halt progression and preserve your vision.
What is Keratoconus? The Basics Every Patient Should Know
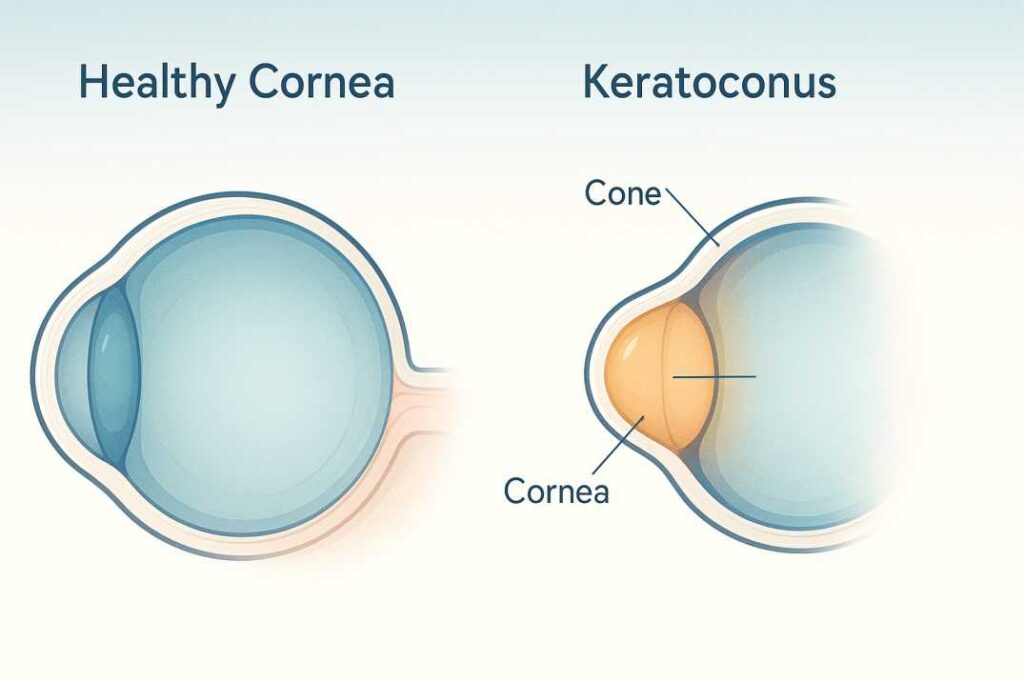
Keratoconus is a progressive bilateral corneal ectatic disorder characterized by cone-like steepening of the cornea, the clear front surface of your eye. EyeWikiNCBI Think of your cornea as the clear window at the front of your eye—normally dome-shaped like a basketball. In keratoconus, the collagen bundles within your cornea become affected, causing the cornea to become weaker and thinner nearer its center or just off-center, leading to an outward bulging that creates an irregular cone-like shape. Keratoconus – information, causes and treatment | RNIB
This disorder is one of the leading indications for corneal transplantation in Western countries and typically manifests during puberty or early adulthood. Keratoconus – StatPearls – NCBI Bookshelf. However, there’s hopeful news: thanks to modern treatment advances, many patients can now avoid transplant surgery entirely through early detection and intervention.
The Historical Understanding
While German professor Burchard Mauchart first described keratoconus in 1748 (referring to it as staphyloma diaphanum), it was in 1854 that Dr. John Nottingham, a British physician, offered comprehensive insight into the condition, and in 1869, John Horner, a Swiss physician, gave it the term “keratoconus.”
How Common is Keratoconus?
Recent research has dramatically revised our understanding of keratoconus prevalence. A comprehensive 2025 systematic review and meta-analysis found the global prevalence of keratoconus is now estimated at 289.1 per 100,000 persons (approximately 1 in 345 people)—more than double earlier estimates. Keratoconus Prevalence Is Rising Worldwide – Optometry Advisor Studies using advanced Scheimpflug imaging technology have revealed prevalence rates approximately ten times higher than the traditional 1986 estimate of 1 in 2,000, with a 2023 German study finding rates of 0.49% in a mainly Caucasian population. Keratoconus Prevalence Tenfold Higher Than Previously Reported. The increase reflects both better diagnostic technology and greater awareness of the condition.
Globally, keratoconus affects 1.38 per 1,000 individuals, with Asian and Middle Eastern populations displaying an earlier onset and more severe symptoms.
Men have slightly higher odds of developing keratoconus compared with women (odds ratio 1.10), though this varies by age group and population. Keratoconus Prevalence Is Rising Worldwide – Optometry Advisor. In the United States, keratoconus is most prevalent in individuals 18 to 39 years of age, with higher prevalence observed in the Black population. Prevalence and Economic Burden of Keratoconus in the United States – PubMed
Recognizing the Signs: Symptoms of Keratoconus
Early detection is crucial for optimal outcomes. At West Broward Eyecare Associates, we emphasize the importance of recognizing these warning signs:
Early-Stage Symptoms
Initially, keratoconus may lead to rapidly worsening refractive error and inability to attain full correction with spectacles. The Latest in Keratoconus Treatment | Ophthalmology Management. Many patients experience:
- Progressive vision blur that glasses can’t fully correct
- Frequent prescription changes (every few months rather than years)
- Increased sensitivity to light and glare (photophobia)
- Difficulty seeing at night with halos or starbursts around lights
- Eye strain and headaches from trying to focus
- Double vision in one eye (monocular diplopia)
- Distorted or wavy vision, making straight lines appear bent
Advanced-Stage Indicators
The disease is characterized by increased sensitivity to light, eye irritation, and blurred vision, and can result in complications such as corneal scarring and irregular astigmatism.
More advanced signs include:
- Munson’s sign: When looking down, the conical shape of the cornea is outlined by the lower eyelid, a sign of severe keratoconus.
- Fleischer’s ring: Iron deposits in the cornea a visible during slit lamp examination.
- Vogt’s striae: Whitish lines in the deep corneal stroma and Descemet’s membrane.
- Corneal hydrops: A break in Descemet membrane allows aqueous to enter the stroma, causing severe corneal thickening, decreased vision, light sensitivity, tearing, and pain. Keratoconus – EyeWiki
What Causes Keratoconus? Understanding Risk Factors
Although keratoconus has been studied for decades, it remains poorly understood. The definitive cause is unknown, though it is believed that the predisposition to develop the disease is present at birth. Keratoconus | Johns Hopkins Medicine A common finding in keratoconus is the loss of collagen in the cornea, which may be caused by some imbalance between production and destruction of corneal tissue by corneal cells. Keratoconus | Johns Hopkins Medicine
Primary Risk Factors
On multivariable analysis, eye rubbing (odds ratio: 4.93), family history of keratoconus (odds ratio: 25.52), and parental consanguinity (odds ratio: 2.89) emerged as significant risk factors for disease development. Risk Factors for Development of Keratoconus: A Matched Pair Case-Control Study – PMC
1. Eye Rubbing: The Modifiable Risk
Mechanical trauma from aggressive or prolonged eye rubbing can contribute to keratoconus development, with correlations between the intensity or frequency of eye rubbing and the disease. Frontiers Eye rubbing, often in the context of ocular allergy, is the main underlying predisposing factor for the development and progression of keratoconus. Frontiers | Management of keratoconus: an updated review
Why does eye rubbing matter so much? Every time you vigorously rub your eyes, you’re applying mechanical pressure to an already vulnerable cornea. For people with a genetic predisposition, this repeated trauma can accelerate corneal thinning and distortion.
2. Genetic Predisposition
Family history of keratoconus increases the risk by 25 times, and patients with a family history of keratoconus or with certain systemic disorders, such as Down syndrome, are at higher risk. PubMed CentralJohns Hopkins Medicine Research shows that a person’s genes can play a major role in developing keratoconus, affecting men and women equally, but being more common in non-Caucasian people. Keratoconus – information, causes and treatment | RNIB
If you have a close family member with keratoconus, we strongly recommend comprehensive corneal screening, even if you’re not experiencing symptoms.
3. Chronic Eye Inflammation
Constant inflammation from allergies or irritants can contribute to the destruction of corneal tissue that may result in the development of keratoconus. Keratoconus | Johns Hopkins Medicine Major risk factors include a history of atopy (allergy, asthma, and eczema). Keratoconus Diagnosis and Treatment: Recent Advances and Future Directions – PMC
Associated Conditions
Environmental risk factors that may play a role include contact lens use, repeated eye-rubbing, or atopy (conditions involving hypersensitivity reactions such as hay fever, eczema, sleep apnea, or allergic asthma). Keratoconus – Symptoms, Causes, Treatment | NORD
Modern Diagnosis: How We Detect Keratoconus
At West Broward Eyecare Associates, we use state-of-the-art diagnostic technology to detect keratoconus early, when treatment is most effective.
Comprehensive Diagnostic Approach
Corneal Topography
Corneal topography is the most accurate way to diagnose early keratoconus and follow its progression, creating a computerized map of the curve of the cornea that can detect early changes before signs and symptoms become more noticeable. EyesflJohns Hopkins Medicine
Corneal Tomography
Corneal tomography allows for three-dimensional visualization of the anterior and posterior corneal surfaces, along with assessment of corneal thickness, emerging as a promising screening tool in the identification of candidates for early corneal collagen cross-linking. Keratoconus Diagnosis and Treatment: Recent Advances and Future Directions – PMC
Optical Coherence Tomography (OCT)
OCT provides detailed images of the cornea’s layers, helping doctors spot thinning or irregularities associated with keratoconus.
Corneal Biomechanics Assessment
Reduced corneal hysteresis reflects the viscoelastic response of the cornea to mechanical stress and has been associated with biomechanical weakening, serving as an early indicator of ectatic changes. Machine learning-assisted early detection of keratoconus: a comparative analysis of corneal topography and biomechanical data – PM.C
Pachymetry
This test measures corneal thickness, essential for confirming the diagnosis of keratoconus, as the condition often causes thinning of the cornea.
Emerging Detection Technologies
Machine learning algorithms, particularly Random Forest, can effectively aid in the early detection of keratoconus in young individuals, with studies achieving accuracy rates of 96-98% on test sets. PubMed Central Natu. These AI-powered tools represent the future of keratoconus screening, allowing for even earlier intervention.
Modern Treatment Options: From Conservative to Advanced
The treatment landscape for keratoconus has been revolutionized in recent years. Thanks to recent advancements, keratoconus is no longer a condition that patients must live with until they progress to transplant surgery. Ophthalmology Management June 2025: THE LATEST IN KERATOCONUS TREATMENT
Early-Stage Treatment Options
Corrective Lenses
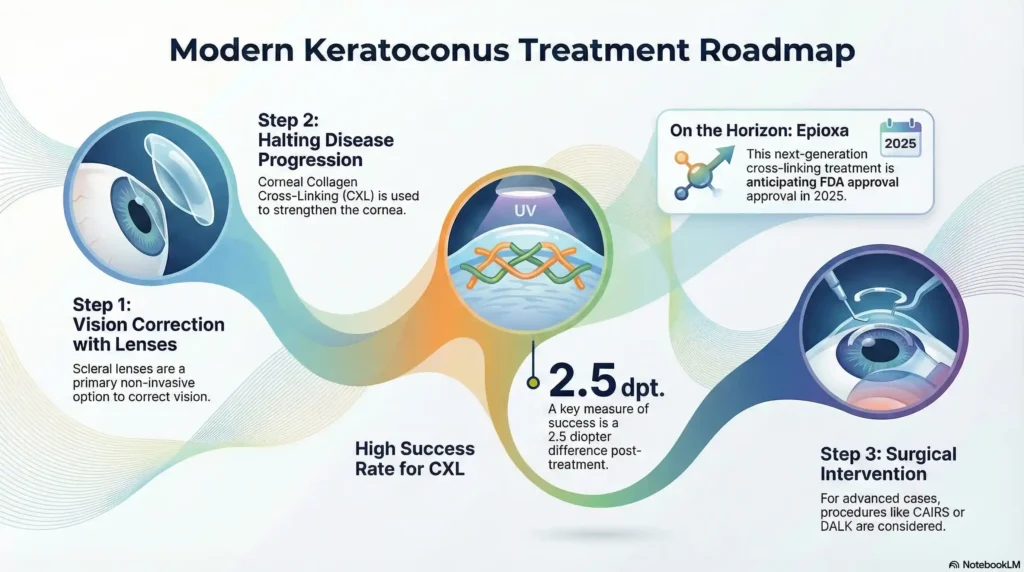
Early stages of keratoconus can be treated with glasses and soft contact lenses, but as it progresses, hard contact lenses, including Rigid Gas Permeable or Scleral Lenses, may be needed. The Eye Condition You Probably Never Heard Of: Keratoconus | Eye Specialists of Mid Florida Scleral lenses vault over the cornea, allowing for better refraction of light onto the retina to create clearer images, and have improved to the point that almost any keratoconus patient can be fitted. The Latest in Keratoconus Treatment | Ophthalmology Management
Why scleral lenses work so well: These large-diameter lenses rest on the white part of your eye (sclera) rather than the cornea itself, creating a smooth optical surface over the irregular cornea while providing exceptional comfort.
Corneal Collagen Cross-Linking (CXL): The Gold Standard
For the limitation of progression, corneal crosslinking has become the gold standard, first approved in the United States in 2016 using the epithelial-off Dresden Protocol. The Latest in Keratoconus Treatment | Ophthalmology Management
How CXL Works
The procedure involves the application of riboflavin (vitamin B2) solution to the eye, which is then activated by ultraviolet light for about 30 minutes or less. The solution causes new collagen bonds to form, recovering and preserving some of the cornea’s strength and shape. Jryneyeclinic – Johns Hopkins Medicine
Think of it as “spot welding” your corneal collagen fibers—creating new bonds that stabilize the structure and prevent further bulging.
Clinical Effectiveness
In pivotal clinical trials, when comparing treated patients to those receiving sham treatment, there was found to be a greater than 2.5 diopter difference in change of maximum K reading (Kmax), favoring the treatment group after 12 months—the treated arm showed greater than 1.5 diopters of flattening, while the sham arm steepened by 1.0 diopters. The Latest in Keratoconus Treatment | Ophthalmology Management
Recovery and Results
You may experience some side effects such as pain, sensitivity to light, dry eye, blurry vision, infection, or scarring. Your vision will be very blurry at first, but should gradually improve within two to three weeks. Keratoconus | Johns Hopkins Medicine
Most patients can return to work within a week, though complete visual recovery may take several months. The discomfort is temporary, but the benefits—halting progression—can last a lifetime.
[Schedule a Keratoconus Screening in Tamarac]
Breakthrough: Transepithelial CXL (Epioxa)
In February 2025, the FDA accepted the New Drug Application for Epioxa, a non-invasive corneal cross-linking therapy that does not require removal of the corneal epithelium, with a target action date of October 20, 2025. FDA Accepts NDA for Epioxa for Keratoconus Treatment | HCPLive Phase 3 trials showed Epioxa significantly improved maximum corneal curvature, meeting primary efficacy endpoints with a Kmax treatment effect of –1.0 D, with the treatment being well-tolerated and most adverse events mild and transient. FDA Accepts NDA for Epioxa for Keratoconus Treatment | HCPLive
What makes Epioxa revolutionary? Traditional CXL requires removing the outer layer of the cornea (epithelium), which causes significant discomfort and requires several days of recovery. Epioxa penetrates through the intact epithelium, potentially offering comparable effectiveness with dramatically improved comfort and faster recovery.
Intracorneal Ring Segments (ICRS)
Intracorneal ring segments improve corneal shape and refractive errors, enhancing visual acuity and potentially quality of life. Keratoconus and quality of life: an updated comprehensive review – PMC. These tiny plastic arcs are inserted into the cornea to help flatten the cone and improve vision, often used in combination with CXL for optimal results.
Advanced Surgical Options: CAIRS
CAIRS (corneal allogenic intrastromal ring segments) is a procedure involving the implantation of arc-shaped segments of donor corneal tissue into the patient’s cornea to reshape it—much less invasive than transplantation, with much less risk, and the segments are removable if needed. PentaVision Ophthalmology Management
When Transplantation is Necessary
Corneal transplant is a surgical procedure reserved for individuals with severe disease (e.g., the cornea is extremely thin and/or vision is significantly compromised) or who cannot tolerate or did not respond to more conservative treatments. NORD PubMed Central
Types of Transplants
- Deep Anterior Lamellar Keratoplasty (DALK): Replaces only the damaged layers, preserving your healthy endothelium
- Bowman Layer Transplantation: Targeted layer replacement for specific cases
- Penetrating Keratoplasty (PK): Full-thickness corneal replacement for advanced disease
The good news? With early detection and modern treatments like CXL, most patients never reach the point of needing a transplant.
Recent Scientific Breakthroughs Supporting Modern Treatment
Study 1: Machine Learning for Early Detection (2024)
A study conducted at the Medical University of Lublin between March and August 2024 found that the Random Forest algorithm demonstrated an accuracy of 98% during training and 96% on the test set for detecting keratoconus, while also identifying the most diagnostically relevant measurements. Machine learning-assisted early detection of keratoconus: a comparative analysis of corneal topography and biomechanical data | Scientific Reports. This research demonstrates how artificial intelligence is revolutionizing early keratoconus detection, allowing for intervention before significant vision loss occurs.
Study 2: Quality of Life Impact Research (2024-2025)
A comprehensive review examining the impact of keratoconus on patients’ quality of life found that the condition profoundly impacts vision-related quality of life beyond reduced visual acuity alone, with multiple factors contributing, including refractive errors, decreased contrast sensitivity, ocular pain and discomfort, and associated comorbidities. Keratoconus and quality of life: an updated comprehensive review – PMC Understanding these impacts helps us provide more comprehensive, patient-centered care.
Study 3: Awareness and Prevention Study (2025)
Research published in 2025 found that 66.6% of participants reported rubbing their eyes, with participants identifying keratoconus risk factors as allergies (30.9%), family history (45%), and sunlight exposure (22.8%), emphasizing the importance of public education regarding early treatment of allergic eye conditions and refraining from eye rubbing to prevent new cases.
Living with Keratoconus: Practical Management Strategies
Lifestyle Modifications That Matter
Patients are advised to avoid eye rubbing and adopt protective measures such as wearing sunglasses outdoors, which can reduce the risk of disease progression. Keratoconus – StatPearls – NCBI Bookshelf
Daily Eye Care Practices
- Stop Eye Rubbing: The single most important modifiable risk factor. When your eyes itch, use preservative-free artificial tears instead of rubbing.
- Manage Allergies: Studies have shown that good control of ocular allergy can reduce the risk of disease progression, development of acute hydrops, and post-keratoplasty complications. Frontiers | Management of keratoconus: an updated review. Work with us to find effective allergy management strategies.
- Protective Eyewear: UV protection is essential. Quality sunglasses aren’t just about comfort—they’re about protecting your corneal health.
- Proper Contact Lens Hygiene: For those wearing corrective lenses, meticulous hygiene prevents complications and ensures optimal vision.
- Regular Monitoring: Follow-up appointments every 3-6 months allow us to track any progression and adjust treatment promptly.
When to Seek Immediate Care
Contact West Broward Eyecare Associates immediately if you experience:
- Sudden vision loss or significant vision change
- Severe eye pain that doesn’t improve
- Signs of corneal hydrops (sudden swelling, severe pain, dramatic vision decrease)
- Eye trauma
- Inability to remove contact lenses
- Severe light sensitivity with discharge
The West Broward Eyecare Associates Advantage
At West Broward Eyecare Associates, we combine cutting-edge technology with compassionate, family-centered care. Our approach to keratoconus includes:
Advanced Diagnostic Technology
State-of-the-art corneal topography, tomography, and biomechanical assessment ensure we catch keratoconus at its earliest stages.
Comprehensive Treatment Options
From specialty contact lenses to the latest cross-linking procedures, we offer the full spectrum of keratoconus care under one roof.
Personalized Care Plans
Your treatment is tailored to your specific condition, lifestyle, and goals. We don’t believe in one-size-fits-all approaches.
Family-Focused Approach
We care for all ages, from pediatric screenings to adult management, because keratoconus often runs in families.
Ongoing Monitoring
Regular follow-ups track progression and allow us to adjust treatment promptly, maximizing your long-term outcomes.
Why Early Detection Matters
Early detection of keratoconus is tantamount to its proper treatment, as timely intervention with progression prevention strategies, such as corneal collagen cross-linking, may help avoid more invasive treatments, such as full or partial thickness corneal transplantation. Keratoconus Diagnosis and Treatment: Recent Advances and Future Directions – PMC
The difference between catching keratoconus early versus late can be the difference between a simple 30-minute procedure and needing a corneal transplant. That’s why we emphasize comprehensive eye exams for anyone with risk factors.
Hope for the Future: Emerging Treatments
The future of keratoconus treatment continues to evolve:
IVMED-80 (Copper Sulfate Eye Drops)
IVMED-80, currently undergoing Phase III FDA trials, was developed to increase lysyl oxidase, a cross-linking enzyme that, when decreased, is linked to keratoconus. What’s on the Horizon for Keratoconu? This pharmaceutical approach could offer non-invasive treatment through simple eye drops.
Regenerative Therapies
Regenerative or cell therapy offers promising treatment options for keratoconus in certain cases. Advances in keratoconus treatment, Stem cell research, and tissue engineering may one day allow us to regenerate damaged corneal tissue.
AI-Assisted Personalized Treatment
Machine learning continues to advance, promising even earlier detection and more personalized treatment protocols based on your individual corneal characteristics, genetic profile, and progression patterns.
Scientific Resources & Further Reading
The information in this comprehensive guide is based on the latest peer-reviewed research and clinical evidence. Below are key scientific resources that informed this article:
1. Machine Learning-Assisted Early Detection of Keratoconus (2025)
Study: “Machine learning-assisted early detection of keratoconus: a comparative analysis of corneal topography and biomechanical data”
Published: Scientific Reports, July 2025
Key Finding: This groundbreaking study from the Medical University of Lublin demonstrated that Random Forest machine learning algorithms achieved 98% accuracy during training and 96% on test sets for detecting keratoconus. The research analyzed 148 corneal scans (72 healthy eyes and 76 keratoconus eyes) and identified the most diagnostically relevant measurements for early detection.
Why It Matters: This research represents a significant advancement in artificial intelligence applications for keratoconus screening, enabling earlier intervention before significant vision loss occurs. The study’s interpretability provides a clinically meaningful bridge between AI-driven predictions and expert-based decision-making.
Access: Nature Scientific Reports – Machine Learning Keratoconus Detection
2. Global Keratoconus Prevalence Meta-Analysis (2025)
Study: “Global incidence and prevalence of keratoconus: a systematic review and meta-analysis”
Published: Cornea, August 2025
Authors: Sriranganathan A, Chan CC, Dhillon J, Felfeli T
Key Finding: This comprehensive systematic review analyzed 55 studies and found the pooled global prevalence of keratoconus is 289.1 per 100,000 persons (approximately 0.29% or 1 in 345 people)—representing more than double the prevalence reported in a 2020 meta-analysis. The study also confirmed that men have slightly higher odds (OR 1.10) of keratoconus, with the highest prevalence and incidence observed in individuals aged 20-29 years.
Why It Matters: This is the most current and comprehensive epidemiological data on keratoconus worldwide, dramatically revising our understanding of how common this condition is. The increased prevalence reflects both improved diagnostic technology and greater clinical awareness, emphasizing the importance of regular eye examinations and early screening.
Reference: Optometry Advisor coverage of the study can be found at: Keratoconus Global Burden Analysis
3. FDA Approval Status of Next-Generation Cross-Linking (2025)
Announcement: “FDA Accepts NDA for Epioxa for Keratoconus Treatment”
Published: February 24, 2025, by Glaukos Corporation
Key Information: The FDA accepted the New Drug Application (NDA) for Epioxa, a transepithelial (epi-on) corneal cross-linking therapy, with a PDUFA target action date of October 20, 2025. Phase 3 pivotal trials demonstrated a clinically meaningful Kmax treatment effect of -1.0 diopter (p <0.0001) at 12 months compared to placebo, with favorable safety and tolerability profiles.
Why It Matters: If approved, Epioxa would become the first FDA-approved non-invasive corneal cross-linking therapy that does not require removal of the corneal epithelium. This advancement promises to reduce procedure times, improve patient comfort, and shorten recovery periods compared to current epithelium-off procedures, potentially transforming the treatment paradigm for keratoconus patients.
Access: HCPLive – FDA Accepts Epioxa NDA
Additional Authoritative Resources
For readers seeking additional information about keratoconus, the following resources provide comprehensive, evidence-based information:
- National Keratoconus Foundation (NKCF): www.nkcf.org – Patient education, clinical trial information, and community support
- American Academy of Ophthalmology – EyeWiki: Comprehensive clinical resource on keratoconus diagnosis and management
- StatPearls – Keratoconus: Updated April 2024, NCBI Bookshelf – Detailed medical reference for healthcare professionals
Take Action: Your Next Steps
If you’re experiencing vision changes or have risk factors for keratoconus, don’t wait. Early intervention offers the best outcomes.
Schedule Your Comprehensive Eye Exam Today
At West Broward Eyecare Associates, we’re here to protect and preserve your vision through every stage of life. Our experienced team provides:
✓ Thorough diagnostic evaluations using the latest technology
✓ Expert treatment recommendations based on current research
✓ Ongoing support and monitoring throughout your care journey
✓ Insurance guidance and flexible payment options
✓ Compassionate care for the whole family
Bottom Line: Expert Care When You Need It Most
Keratoconus is a serious but highly manageable condition. With modern diagnostic tools and treatment options available in 2025, most patients can maintain excellent vision and quality of life. The key is early detection and appropriate intervention.
Keratoconus is no longer a condition that patients must live with until they progress to transplant surgery—with proper management, progression can be slowed or halted completely. Ophthalmology Management June 2025: THE LATEST IN KERATOCONUS TREATMENT
Your vision is precious. Whether you’re newly diagnosed, managing established keratoconus, or concerned about family risk factors, West Broward Eyecare Associates is here as your trusted partner in comprehensive eye health.
Remember: Understanding the condition, the importance of regular monitoring, lifestyle modifications, and comprehensive patient education can significantly contribute to maintaining visual function and quality of life. Keratoconus – StatPearls – NCBI Bookshelf
Don’t let keratoconus control your life—take control of your vision health today. Call us to schedule your comprehensive keratoconus evaluation.
Note to Readers: Medical research is constantly evolving. The studies cited in this article represent the most current evidence available as of October 2025. Always consult with a qualified eye care professional at West Broward Eyecare Associates for personalized medical advice and the most up-to-date treatment options for your specific condition.
FAQs
-
Keratoconus causes the cornea to thin and bulge into a cone shape, leading to blurry vision, glare, and sensitivity to light.