Myopia in Children: Early Detection & Management Guide 2025
The childhood myopia epidemic has reached alarming proportions, with nearly one-third of children globally now affected by nearsightedness. Early detection and proactive management strategies can slow progression by up to 60%, protecting your child’s long-term vision health.
Understanding Myopia in Children: The Growing Crisis
Myopia, commonly known as nearsightedness, has transformed from a simple vision correction need into a global public health crisis. This refractive condition occurs when the eyeball elongates beyond normal proportions, causing light rays to focus in front of the retina rather than directly on it. The result: distant objects appear blurry while nearby items remain clear.
The Alarming Statistics
The numbers paint a concerning picture for our children’s future vision health:
- Global Impact: The global prevalence of childhood myopia is substantial, affecting approximately one-third of children and adolescents, with notable variations in prevalence across different demographic groups
- Rising Trend: Short-sightedness in children tripled between 1990 and 2023, and the increase was ‘particularly notable’ after the COVID-19 pandemic
- Future Projections: It is anticipated that the global incidence of myopia will exceed 740 million cases by 2050
Why This Matters More Than Ever
Unlike previous generations, where myopia was primarily seen as an inconvenience requiring glasses, today’s understanding reveals serious long-term consequences. Between 5% and 15% of people with myopia have severe myopia, also called high myopia. This puts them at a higher risk of eye complications later in life that could affect their vision and even cause blindness.
The complications associated with high myopia include:
- Retinal detachment
- Glaucoma
- Myopic maculopathy
- Cataracts
- Choroidal neovascularization
Early Warning Signs Every Parent Should Know
Recognizing the early signs of myopia in children is crucial for timely intervention. Many children don’t realize their vision is changing, making parental observation essential.
Behavioral Changes to Watch For
Academic Performance Indicators:
- Difficulty seeing the classroom board
- Squinting when looking at distant objects
- Moving closer to the television or computer screen
- Holding books or devices very close to their face
Physical Signs:
- Frequent eye rubbing
- Excessive blinking
- Complaints of headaches, especially after school
- Eye fatigue or strain after visual tasks
Social and Activity Changes:
- Reluctance to participate in sports or outdoor activities
- Difficulty recognizing faces from a distance
- Complaints about not being able to see clearly during activities
Age-Specific Considerations
Preschool Age (3-5 years):
- Limited attention span during visual activities
- Difficulty with fine motor tasks requiring vision
- Unusual head tilting or posturing
School Age (6-12 years):
- Declining academic performance
- Increased complaints about classroom visibility
- Preference for near activities over distant ones
Adolescents (13-18 years):
- Difficulty with driving preparation
- Sports performance issues
- Self-reported vision changes
The Critical Importance of Early Detection
Early detection of myopia isn’t just about getting glasses—it’s about preventing a lifetime of vision complications. Early detection and proactive management of myopia in children are essential to ensure long-term vision health. Regular eye exams and effective myopia management strategies can prevent myopia progression and reduce the risk of serious eye conditions.
The Science Behind Early Intervention
Recent research has revolutionized our understanding of when and how to intervene:
Pre-Myopia Detection: Pre-myopia, defined by an inadequate hyperopic reserve, increases myopia risk in childhood. Children with insufficient hyperopic reserve (typically less than +0.75D) are at significantly higher risk of developing myopia.
The Window of Opportunity: The 2025 guidelines prioritize delaying myopia onset as a key preventive strategy, with even short delays offering benefits. Every month that myopia onset can be delayed reduces the lifetime risk of high myopia and associated complications.
Recommended Screening Schedule
Based on current guidelines from leading pediatric eye care organizations:
Ages 6 months – 2 years:
- Initial comprehensive eye examination
- Assessment for refractive errors and eye alignment
Ages 3-5 years:
- Annual vision screenings
- Pre-school comprehensive eye exam
- Baseline refractive measurements
School age and beyond:
- Annual comprehensive eye examinations
- Biannual monitoring for myopia is conducted
- Axial length measurements for progression tracking
Evidence-Based Management Strategies
Modern myopia management goes far beyond simply prescribing stronger glasses each year. Today’s evidence-based approaches can slow progression by 30-60%, dramatically reducing the risk of high myopia and associated complications.
The Paradigm Shift in Treatment
Traditional methods of myopia management, such as corrective lenses and refractive surgery, restore clear distance vision but do not slow axial elongation and, hence, myopia-associated risks. Interests and efforts in developing myopia control treatments have intensified in recent years.
Core Management Principles
1. Comprehensive Assessment Every child with myopia should receive:
- Detailed refractive history
- Axial length measurements
- Parental myopia assessment
- Lifestyle and environmental evaluation
- Discussion of treatment goals and expectations
2. Individualized Treatment Planning Treatment selection considers:
- Child’s age and cooperation level
- Rate of myopia progression
- Lifestyle and activity preferences
- Family preferences and practical considerations
- Risk factors for rapid progression
3. Regular Monitoring and Adjustment. Successful myopia management requires:
- Regular follow-up appointments (every 6 months minimum)
- Ongoing assessment of treatment efficacy
- Adjustment of interventions based on progression rates
- Long-term commitment to treatment protocols
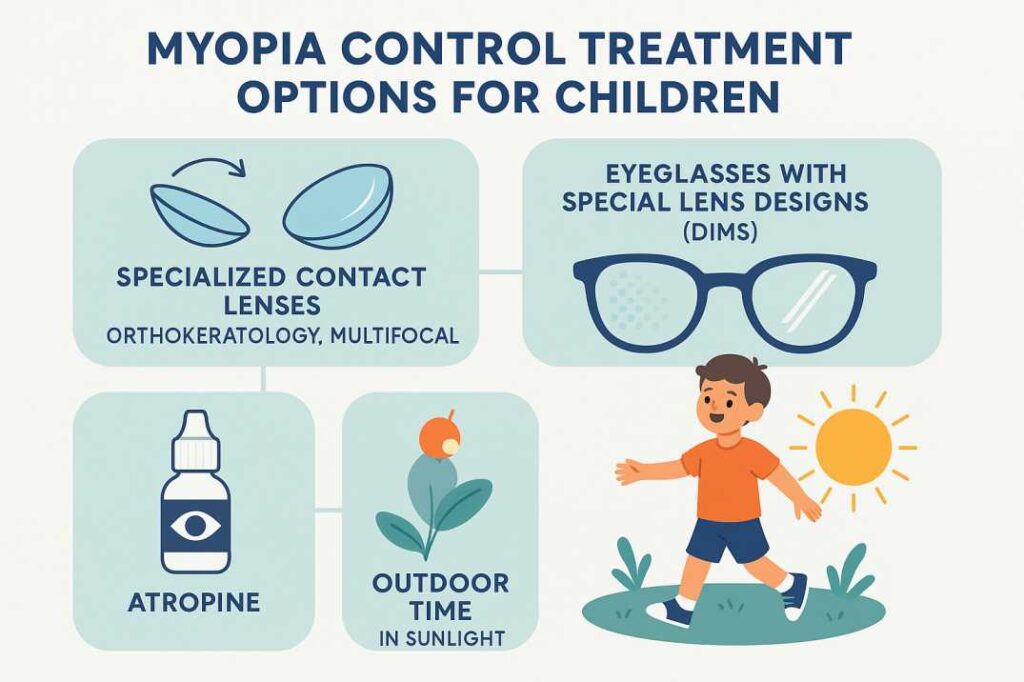
Cutting-Edge Treatment Options for 2025
The field of myopia control has exploded with innovative treatment options, each with unique mechanisms and benefits.
Optical Interventions
Orthokeratology (Ortho-K). In two distinct randomized controlled studies, the Retardation of Myopia in Orthokeratology (ROMIO) study by Cho et al., and the HM-PRO trial by Charm and Cho, a reduction of axial elongation ranging from 43 to 63% was detected.
How it works: Special rigid contact lenses worn overnight temporarily reshape the cornea, providing clear daytime vision without glasses or contacts while slowing eye growth.
Best for: Children 8+ years old with moderate myopia who are comfortable with contact lens care.
Multifocal Contact Lenses Studies have shown that wearing multifocal contact lenses can also help slow down the progression of myopia in children and teenagers. These contact lenses have different zones to correct near and distance sight simultaneously.
How it works: These specialized lenses create peripheral myopic defocus, which signals the eye to slow its growth.
Best for: Older children and teens who can handle daily contact lens wear.
Specialized Spectacle Lenses DIMS lenses incorporate a central zone for clear vision surrounded by annular segments that provide constant myopic defocus. A two-year randomised trial in Hong Kong demonstrated a 52% reduction in myopia progression and a 62% reduction in axial elongation with DIMS lenses.
How it works: Advanced lens designs create specific defocus patterns that slow eye growth while maintaining clear central vision.
Best for: Younger children or those who prefer glasses over contact lenses.
Pharmacological Treatments
Low-Dose Atropine Eye Drops Low-dose atropine eye drops have shown 30 to 60% efficacy in slowing myopia progression in children, while specialized lenses (e.g., multifocal contacts, orthokeratology) similarly reduce progression rates by 40 to 60% on average.
How it works: Atropine affects biochemical pathways that control eye growth, with minimal side effects at low concentrations.
Best for: Children 4+ years old, often used in combination with optical treatments.
Emerging Therapies
Repeated Low-Level Red-Light (RLRL) Therapy. RLRL therapy represents a novel, non-invasive option with growing support. This cutting-edge treatment uses specific wavelengths of red light administered in brief daily sessions.
How it works: Low-intensity red light appears to modulate cellular activity in ways that slow eye growth.
Best for: Children who may not tolerate other interventions well.
Combination Approaches
Increasingly, clinicians are moving toward personalised, multimodal approaches, combining therapies such as low-dose atropine with Ortho-K or MFCLs to enhance efficacy. These combinations have shown additive benefits in several studies, particularly for children with high baseline risk or rapid progression.
Popular combinations include:
- Ortho-K + low-dose atropine
- Multifocal contact lenses + atropine
- Specialized spectacles + environmental modifications
Prevention: Building Healthy Vision Habits
While genetics plays a role in myopia development, environmental factors are increasingly recognized as the primary drivers of the current epidemic. This means parents have significant power to influence their child’s vision outcomes.
The Outdoor Advantage
Time spent outdoors seems to help prevent the onset of myopia, but unfortunately, it does not affect the condition’s progression, which highlights the importance of early detection.
Recommended Outdoor Time:
- Minimum: 2 hours daily for young children
- Optimal: 2-3 hours during peak sunlight hours
- Quality matters: Bright outdoor light (>1000 lux) is more protective than indoor activities
Practical Implementation:
- Schedule outdoor recess and lunch periods at school
- Encourage after-school outdoor play
- Family outdoor activities on weekends
- Sports participation in outdoor venues
- Walking or biking to school when possible
Managing Screen Time and Near Work
The COVID-19 pandemic has caused people to rely more on digital devices due to lockdown measures, which has led to concerns about the potential increased risk of myopia.
Evidence-Based Guidelines:
- Follow the 20-20-20 rule: Every 20 minutes, look at something 20 feet away for 20 seconds
- Maintain proper reading distance (at least 30-40 cm from books/screens)
- Ensure adequate lighting for near work
- Take regular breaks from continuous near activities
- Limit recreational screen time according to age-appropriate guidelines
Environmental Optimization
Home Environment:
- Maximize natural light in study areas
- Position desks near windows when possible
- Use adjustable task lighting for homework
- Create designated screen-free zones and times
School Advocacy:
- Advocate for outdoor classroom time when the weather permits
- Support school policies promoting outdoor recess
- Encourage proper classroom lighting
- Promote awareness of myopia prevention among educators
Working with Your Eye Care Provider
Successful myopia management requires a collaborative partnership between families and qualified eye care professionals. Understanding what to expect and how to maximize this relationship is crucial for optimal outcomes.
Choosing the Right Provider
Essential Qualifications:
- Board-certified optometrist or ophthalmologist
- Specialized training in pediatric eye care
- Experience with myopia control treatments
- Access to advanced diagnostic equipment (axial length measurement)
- Commitment to evidence-based practices
Questions to Ask:
- What myopia control options do you offer?
- How do you monitor treatment effectiveness?
- What is your experience with pediatric myopia management?
- How often will my child need follow-up appointments?
- What are the realistic expectations for treatment outcomes?
The Treatment Journey
Initial Consultation:
- Comprehensive eye examination
- Detailed family and medical history
- Lifestyle assessment
- Discussion of treatment options
- Development of a personalized management plan
Ongoing Care:
- Regular monitoring appointments (typically every 6 months)
- Adjustment of treatment protocols as needed
- Assessment of treatment compliance and effectiveness
- Long-term planning for treatment duration
Key Metrics Tracked:
- Refractive error changes
- Axial length progression
- Visual acuity maintenance
- Treatment adherence
- Any side effects or complications
Preparing for Appointments
Information to Bring:
- Previous eye exam records
- Family history of vision problems
- Current symptoms or concerns
- Questions about treatment options
- Insurance information
Questions to Prepare:
- How quickly is my child’s myopia progressing?
- What are the long-term risks if we don’t treat?
- Which treatment option is best for my child’s lifestyle?
- What results can we realistically expect?
- How long will treatment be needed?
Recent Scientific Evidence Supporting Early Intervention
Breakthrough Research Findings
Study 1: Comprehensive Global Meta-Analysis (2025) A 2025 narrative review published in Eye analyzed current and emerging myopia control strategies, confirming that multifocal contact lenses, orthokeratology, and defocus-incorporated spectacles are effective in modulating axial elongation. Low-dose atropine remains a cornerstone pharmacologic therapy with consistent efficacy, and behavioral interventions such as increased outdoor time provide preventive benefits.
Study 2: COVID-19 Impact Assessment (2024) Research published in 2024 documented the pandemic’s impact on childhood myopia, showing approximately a 0.3D increase in myopia progression during 2020 compared to previous years, particularly among younger children aged 6-8 years. The prevalence of myopia detected in 2020 surpassed the highest recorded levels between 2015 and 2019.
Study 3: Atropine Efficacy Research (2025) A comprehensive meta-analysis published in Frontiers in Pharmacology in 2025 specifically examined 0.01% atropine efficacy worldwide, providing updated evidence on concentration-dependent effects and confirming the importance of individualized dosing based on patient response and geographic factors.
Clinical Implications
These studies reinforce several critical points:
-
Multiple effective treatments exist: No single treatment works for all children, but various options provide significant benefits.
-
Early intervention matters: The younger the child when treatment begins, the better the long-term outcomes.
-
Environmental factors are modifiable: Parents and schools can implement changes that meaningfully impact myopia risk.
-
Comprehensive monitoring improves outcomes: Regular assessment using advanced diagnostic tools optimizes treatment effectiveness.
Key Takeaways: Your Child’s Vision Action Plan
Immediate Steps (Next 30 Days)
- Schedule a comprehensive eye exam if your child shows any warning signs
- Increase outdoor time to at least 2 hours daily
- Implement the 20-20-20 rule for screen time
- Document any vision-related behaviors you observe
Medium-Term Goals (3-6 Months)
- Establish a relationship with a qualified pediatric eye care provider
- Develop family vision, health habits around outdoor time, and screen management
- Advocate for outdoor policies at your child’s school
- Monitor and track any changes in your child’s vision or behavior
Long-Term Commitment (Ongoing)
- Maintain regular eye examinations even if no problems are detected
- Stay informed about advances in myopia control research
- Support treatment compliance if myopia control is recommended
- Continue healthy vision habits throughout childhood and adolescence
Emergency Indicators – Seek Immediate Care
- Sudden vision changes
- Eye pain or persistent headaches
- Flashing lights or floating spots
- Any injury to the eye area
Key Scientific References and Citations
Primary Research Sources Used in This Article
1. Global Prevalence and Projection Study (2025) Liang, J., Pu, Y., Chen, J., et al. (2025). Global prevalence, trend, and projection of myopia in children and adolescents from 1990 to 2050: a comprehensive systematic review and meta-analysis. British Journal of Ophthalmology, 109(3), 362-371.
This comprehensive meta-analysis of 276 studies involving 5,410,945 participants from 50 countries provided the current global prevalence data showing myopia in children increased from 24.3% to 35.8% over 30 years, with projections reaching 39.8% by 2050.
Link: https://pubmed.ncbi.nlm.nih.gov/39317432/
2. Current Myopia Control Strategies Review (2025) Maulvi, F.A., Desai, D.T., Kalaiselvan, P., et al. (2025). Current and emerging strategies for myopia control: a narrative review of optical, pharmacological, behavioural, and adjunctive therapies. Eye.
This 2025 narrative review synthesized current evidence on myopia control strategies, confirming that multifocal contact lenses, orthokeratology, and defocus-incorporated spectacles are effective in modulating axial elongation, with low-dose atropine remaining a cornerstone therapy.
Link: https://www.nature.com/articles/s41433-025-03949-1
3. Atropine Efficacy Meta-Analysis (2025) Navarra, P., Buzzonetti, L., Amico, V., et al. (2025). A systematic review with meta-analysis on the efficacy of 0.01% atropine eyedrops in preventing myopia progression in worldwide children’s populations. Frontiers in Pharmacology, 16, 1497667.
This systematic review and meta-analysis specifically examined the efficacy of 0.01% atropine across different global populations, providing crucial evidence on concentration-dependent effects and the importance of individualized dosing approaches for children.
Link: https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1497667/full
Conclusion
Myopia in children represents a significant and growing global health challenge requiring immediate attention from healthcare providers, families, and public health systems. The current evidence strongly supports early detection and intervention strategies that can meaningfully reduce progression rates and prevent sight-threatening complications.
Key Clinical Findings:
- Current global prevalence of 35.8% in pediatric populations, with projections reaching 39.8% by 2050
- Evidence-based interventions can reduce progression by 30-67% when implemented appropriately
- Early intervention (ages 6-8) demonstrates superior efficacy compared to delayed treatment
- Combination therapies show promise for high-risk populations
Clinical Practice Implications: Healthcare providers should implement systematic screening protocols for all children, with particular attention to high-risk populations. Treatment selection should be individualized based on patient age, progression rate, lifestyle factors, and family preferences. Long-term monitoring is essential to ensure treatment efficacy and safety.
Future Directions: Continued research is needed to optimize treatment protocols, develop novel therapeutic approaches, and establish population-based prevention strategies. Public health initiatives focusing on environmental modifications and early detection programs will be crucial for addressing this growing epidemic.
The management of pediatric myopia requires a coordinated, evidence-based approach combining clinical expertise, patient education, and ongoing research to protect children’s vision for life.
Medical Disclaimer: This article is intended for educational and informational purposes only. It does not constitute medical advice and should not replace consultation with qualified healthcare professionals. Individual treatment decisions should always be made in consultation with a licensed ophthalmologist or optometrist experienced in pediatric myopia management. Parents and caregivers should seek professional medical evaluation for any vision concerns in children.
FAQs
-
Early signs include squinting to see distant objects, sitting close to screens, frequent headaches, holding books very close, and complaints of tired eyes.