How COVID-19 Affects Eyes: Symptoms & Risks
How does COVID-19 affect the eyes?
Much has been talked about regarding the wide variety of symptoms associated with the coronavirus disease 2019 (COVID-19). While we are still learning about the various systems in our body that can be affected, we are just beginning to understand how the disease affects the eyes.
Recent research has shown us that the virus is transmitted through respiratory droplets and can be absorbed or spread through the surface of the eye. This is because the eyes are the only area of our body that are completely exposed to the environment (not protected by skin). It is important to be aware of signs that could be associated with COVID-19.
If you’re experiencing any of the following symptoms, schedule an eye exam to have your eyes examined by a professional.
Ocular symptoms that have been reported:
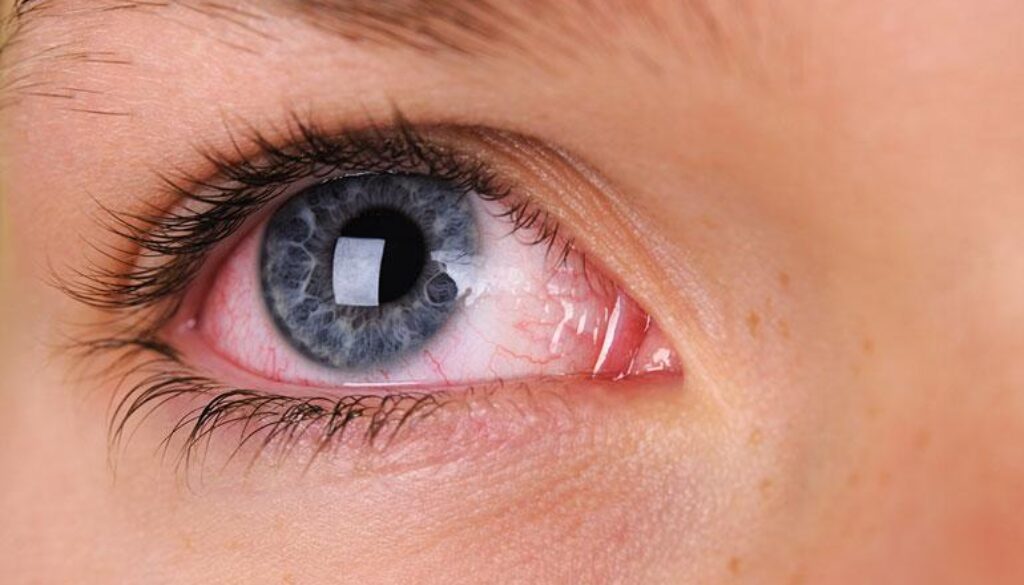
- Red eyes – redness can be due to a viral cause (like COVID-19), bacteria, allergies, dry eyes, or a wide variety of other causes.
- Excessive tearing – may be associated with any inflammation or infection in the eyes. Oftentimes the eyes will tear up because they are trying to remove something irritating them, whether that be an eyelash, allergen, or a virus.
- Others that may be associated: discharge from eyes, eye rubbing in children
What does the Optometrist see if you have COVID-19?
- Conjunctivitis – a general term for inflammation of the conjunctiva, or top layer of the “white” of our eyes.
- Follicles – bumps on the inside of the eyelid, often associated with viral infection
- Epiphora – a clinical term for excessive tearing
- Swollen lymph nodes– the lymphatic system is one of the ways your body helps fight infection. You have nodes in front of your ears and below your jaw that can become swollen with a viral infection.
Long-Term Effects of COVID-19 on Eye Health
While most COVID-19-related eye symptoms resolve within weeks, some Tamarac, FL, patients report lingering issues. Research highlights:
-
Persistent dry eye: Up to 20% of long COVID patients in South Florida experience chronic dryness due to reduced tear production or nerve damage.
-
Retinal changes: Rare vascular complications (e.g., blood clots in retinal veins) may threaten vision if untreated.
-
Optic nerve inflammation: Linked to post-COVID autoimmune responses, causing blurred vision or light sensitivity.
COVID-19 Vaccines and Eye Health
Vaccines remain critical to reducing severe COVID-19 outcomes, including ocular risks. Key facts for Tamarac, FL, patients:
-
No proven link to eye damage: CDC and FDA data confirm vaccines do not cause glaucoma, blindness, or optic neuritis.
-
Rare, temporary reactions: Minor redness or swelling at injection sites near the eyes (e.g., filler-related) resolve quickly.
-
Protection against complications: Vaccinated individuals are less likely to develop COVID-related conjunctivitis or vascular eye issues.
Age-Specific Impacts: Children, Adults, and the Elderly
COVID-19’s ocular effects vary by age group:
-
Children: Higher rates of viral conjunctivitis and eye rubbing. Tamarac parents should watch for:
➔ Watery discharge or crusty eyelids
➔ Frequent squinting or light avoidance -
Adults: Screen time spikes and mask use fuel dry eye. Broward County remote workers benefit from:
➔ Blue-light-blocking glasses
➔ Artificial tears approved by your Coral Springs optometrist -
Elderly: Higher risk of retinal artery occlusion due to COVID-induced inflammation. Annual dilated exams at West Broward Eye are crucial for early detection.
Can COVID-19 Enter Through Your Eyes? Tamarac Eye Protection Guide
Research confirms eyes are potential COVID-19 entry points. The virus can bind to conjunctival membranes and appear in tear film, sometimes causing “pink eye” (conjunctivitis). While less common than nasal transmission, Tamarac residents should consider these protective measures:
-
Avoid Eye Contact
Keep hands away from eyes until thoroughly washed -
Use Protective Barriers
Wear goggles or shields in Tamarac healthcare settings, crowded indoor venues, or when caring for infected individuals -
Prioritize Hand Hygiene
Wash frequently with soap for 20 seconds or use an alcohol-based sanitizer
Pandemic Lifestyle Changes and Eye Strain
Tamarac residents face new eye health challenges:
-
Digital eye strain: 60% of local patients report screen fatigue. Combat it with:
✔️ The 20-20-20 rule (look 20 feet away every 20 minutes)
✔️ Adjusting screen brightness to match ambient light -
Mask-associated dry eye (MADE): Tight-fitting masks redirect breath, drying the eyes. Fixes include:
✔️ Using hypoallergenic tape to seal mask tops
✔️ Preservative-free lubricating drops -
Reduced outdoor time: Less sunlight exposure may worsen myopia in kids. Schedule a pediatric eye exam in Tamarac if their vision seems blurry.
Urgent Eye Symptoms During COVID: When Tamarac Residents Need Immediate Care
While most eye irritation resolves independently, these red flags warrant prompt evaluation at our Tamarac clinic:
Seek Immediate Care For:
-
Severe eye pain or pressure
-
Sudden vision loss or significant blurring
-
Intense redness/swelling of eyelids
-
Persistent discharge with light sensitivity
Your Action Plan:
-
Call (954) 726-0204 for same-day emergency slots
-
Use telemedicine for initial symptom screening
-
Isolate and wear a mask when visiting the clinic
Can it be treated?
There are no treatments for viral eye infections. We can help diagnose and soothe the eyes, as we can only treat symptoms associated. The most important thing is to be evaluated and confirm a diagnosis of viral conjunctivitis to determine if you need to be tested for COVID-19 and isolated.
Reach out to your eye doctor if you think you have irritated, red, watery eyes to be evaluated. Schedule your appointment online or call our office.
FAQs
-
Redness (viral conjunctivitis), excessive tearing, eye discharge, or follicles on the eyelids may indicate COVID-19. Swollen lymph nodes near the ears or jaw can also occur. An optometrist can diagnose viral causes and recommend testing if needed.