Sudden Floaters & Flashes? Get Emergency Eye Care | Tamarac
Sudden eye floaters and flashes can be harmless signs of aging, but they often signal a medical emergency like a retinal tear or detachment. If you are experiencing a “shower” of new specks or a dark curtain over your vision, you require an eye examination within 24 hours to prevent permanent vision loss.
[Request a Same-Day Emergency Appointment]
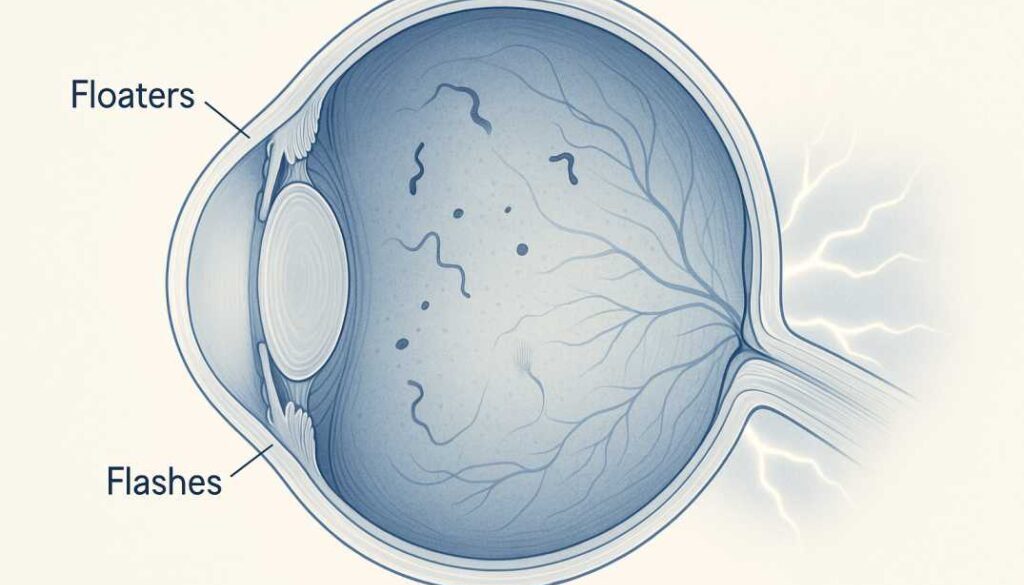
What Are Floaters? More Than Just Annoying Specks
Eye floaters appear as small shapes moving through your field of vision. They might look like tiny dots, squiggly lines, threadlike strands, cobwebs, or even ring-shaped shadows. The medical term for floaters is “myodesopsia,” and what you’re actually seeing isn’t floating debris in front of your eye—it’s shadows cast on your retina by clumps inside your eye.
The Science Behind Floaters
Your eye is filled with a clear, gel-like substance called the vitreous humor, which helps maintain your eye’s round shape and provides a pathway for light to reach the retina. The vitreous is composed of millions of fine fibers intertwined throughout this gel. As you age, this once-firm gel begins to change:
- The vitreous becomes more liquid and less structured
- Tiny protein fibers within the gel clump together
- These clumps cast shadows on the light-sensitive retina at the back of your eye
- Your brain interprets these shadows as floating objects in your vision
Floaters move as your eyes move because they’re literally floating in the vitreous gel. When you try to look directly at them, they seem to dart away—this happens because the movement of your eye causes the vitreous to shift, making the floaters move out of your direct line of sight.
Who Gets Floaters?
Floaters become increasingly common with age. Research shows that about 25% of people experience some vitreous changes with floaters by their 60s, and this rises to approximately two-thirds of people over age 80. However, floaters aren’t limited to older adults.
You’re at higher risk if you:
- Are nearsighted (myopic), especially with prescriptions over -3.00D
- Have had cataract surgery or other eye procedures
- Have experienced eye trauma or injury
- Have diabetes
- Have inflammatory eye conditions like uveitis
- Are between 50-75 years old (when posterior vitreous detachment most commonly occurs)
- Have a family history of retinal problems
Understanding Flashes: When Light Appears From Nowhere
Flashes—medically termed “photopsias”—are brief bursts of light in your vision that can appear as:
- Lightning streaks or bolts
- Bright spots or sparkles
- Camera flash-like bursts
- Short white or golden yellow streaks, typically in peripheral vision
- Arc-shaped flickers
What Causes Flashes?
Flashes occur when the vitreous gel physically tugs, rubs, or bumps against the retina. Your retina is designed to respond to light, but it also reacts to mechanical pressure or stimulation. When the shrinking vitreous pulls on the retina, it triggers the light-sensitive cells, causing your brain to perceive flashes of light even though no actual light is entering your eye.
This is similar to the “stars” you might see if you’ve ever been hit in the eye or head—mechanical stimulation of the retina creates the sensation of seeing light.
Important distinction: Flashes from eye conditions differ from migraine auras, which typically appear as jagged zigzag lines lasting 10-30 minutes and often affecting both eyes simultaneously.
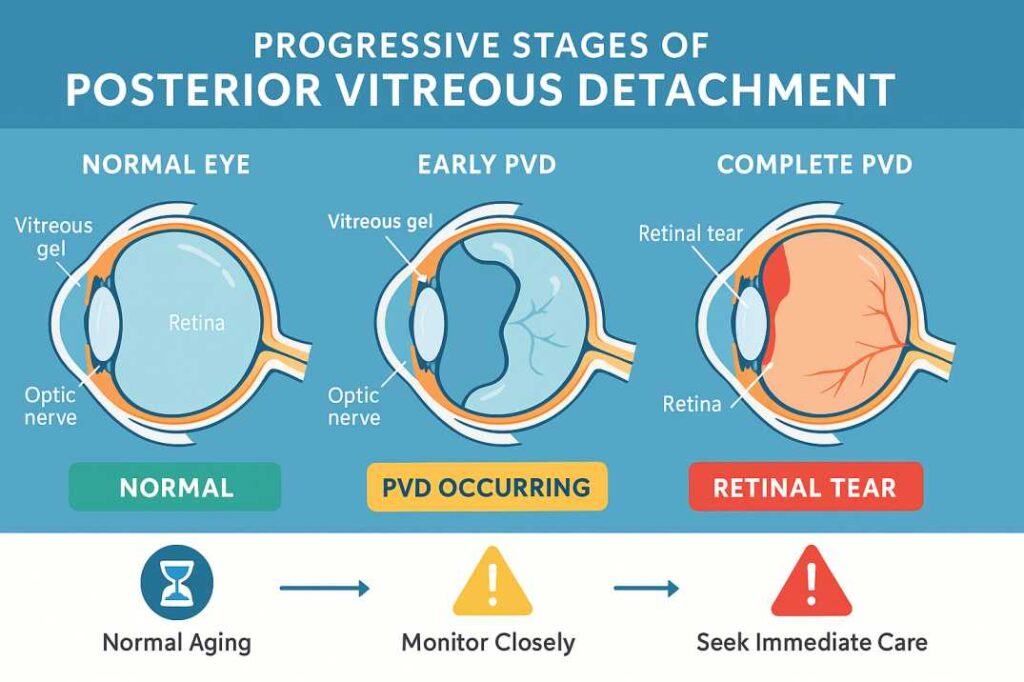
The Aging Process: Posterior Vitreous Detachment (PVD)
The most common cause of floaters and flashes is a natural aging process called posterior vitreous detachment (PVD). This is when the vitreous gel shrinks and pulls away from the retina.
How PVD Develops
When you’re born, the vitreous has a firm, jello-like consistency and is firmly attached to the retina. As you age:
- The vitreous gradually becomes more watery and liquefied
- It begins to shrink and collapse away from the retina
- The delicate fibers that once connected the vitreous to the retina loosen and pull free
- This separation creates floaters (from the debris) and flashes (from the tugging motion)
PVD is extremely common—studies show it affects 24% of adults aged 50-59 and increases to 87% of people over 80. In most cases, this is a benign process that doesn’t threaten your vision.
PVD Timeline and Symptoms
When PVD occurs, you might suddenly notice:
- A large new floater appearing in the center of your vision
- A ring-shaped floater (called a Weiss ring, formed when the vitreous detaches from around the optic nerve)
- Occasional flashes of light, especially in low-light conditions or peripheral vision
- Floaters that are particularly noticeable against bright backgrounds like the sky or white walls
The flashes typically diminish over several weeks or months as the vitreous completely separates from the retina and stops tugging on it. However, floaters may persist long-term, though most people gradually notice them less as their brain adapts.
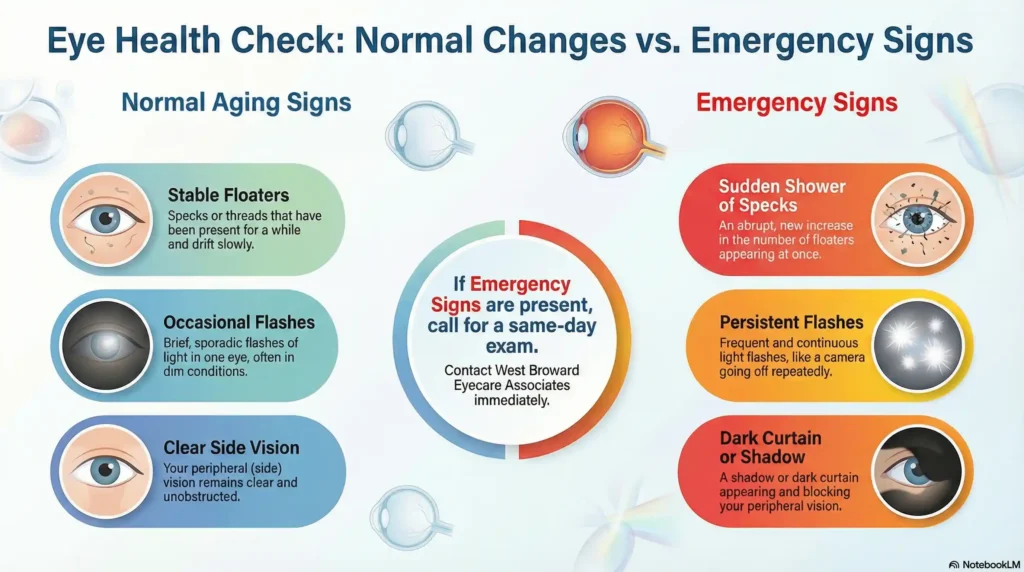
When Floaters and Flashes Become an Emergency: Critical Warning Signs
While most floaters and flashes are harmless, certain symptoms indicate a potential sight-threatening emergency that requires immediate medical attention—within 24 hours or less.
SEEK EMERGENCY EYE CARE IMMEDIATELY IF YOU EXPERIENCE:
Sudden Onset of Multiple New Floaters:
- A sudden “shower” of many tiny black specks appearing all at once
- Hundreds of small dots appearing suddenly (may indicate vitreous hemorrhage)
- Multiple new floaters appearing within hours or days
- Floaters that look like cobwebs or a spider web suddenly appearing in your vision
Dramatic Increase in Flashes:
- Persistent, repeated flashes occurring within seconds or hours of each other
- Flashes that are much more intense or frequent than you’ve experienced before
- Continuous flashing that doesn’t subside
Vision Changes:
- A dark shadow appearing in your peripheral (side) vision
- A “curtain” or “shade” being drawn across your field of vision
- Sudden blurriness or reduced vision
- Loss of part of your visual field
- A gray curtain covering part of your vision
- Central vision becoming suddenly blurry (may indicate macular involvement)
These symptoms together may indicate:
- Retinal tear
- Retinal detachment
- Vitreous hemorrhage
⚠️ DO NOT WAIT: Call your eye doctor immediately or go to the emergency room. Retinal detachment is painless but can cause permanent vision loss if untreated.
Understanding Retinal Tears and Detachment: A Vision-Threatening Emergency
The reason sudden changes in floaters and flashes require urgent attention is the risk of retinal tear and detachment—serious conditions that can lead to permanent vision loss if untreated.
How Retinal Tears Develop
In approximately 14% of PVD cases, the vitreous doesn’t separate cleanly from the retina. Instead:
- The vitreous remains stuck to certain areas of the retina
- As it shrinks and pulls away, it tugs forcefully on these attachment points
- This traction can tear the delicate retinal tissue
- Blood vessels may rupture, causing vitreous hemorrhage (bleeding into the eye)
From Tear to Detachment
A retinal tear is extremely dangerous because:
- Fluid can seep through the tear and accumulate under the retina
- This fluid separates the retina from the nourishing tissue layers beneath it
- Without its blood supply, retinal cells begin to die
- Up to 50% of untreated retinal tears progress to full retinal detachment
- Once vision is lost from retinal detachment, it cannot be fully recovered
Timeline Matters: The Critical Window
Research shows that:
- The risk of retinal tear is highest during the first 4-6 weeks after PVD symptoms begin
- 3.4% of people with uncomplicated PVD will develop a new retinal tear within six weeks
- Same-day evaluation is crucial for anyone experiencing sudden symptoms with visual field defects
- Prompt treatment within 24-48 hours is essential for preserving vision
The good news: When retinal tears are detected early—before full detachment occurs—they can often be treated with a simple in-office laser procedure that can save your vision.
Risk Factors: Who’s Most at Risk for Serious Complications?
While anyone can experience floaters and flashes, certain factors increase your risk of developing sight-threatening complications:
High-Risk Factors:
- High myopia (nearsightedness): People with prescriptions greater than -3.00D have significantly higher risk
- Previous eye surgery: Especially cataract surgery or YAG laser capsulotomy
- Eye trauma or injury: Even injuries that occurred months earlier
- Family history: Genetic predisposition to retinal issues
- Previous retinal tear or detachment in the other eye
- Age 50-75 years: Peak time for PVD occurrence
- Inflammatory eye conditions: Such as uveitis
Medical Conditions:
- Diabetes (increases risk of vitreous changes and hemorrhage)
- High blood pressure (can affect retinal blood vessels)
- Certain connective tissue disorders
- Lattice degeneration (a thinning of the peripheral retina)
Differential Diagnosis: Other Causes of Flashes
Not all flashes are related to eye problems. It’s important to distinguish between different types of visual disturbances:
Migraine with Aura
Some people experience visual disturbances as part of migraine headaches, including:
- Jagged lines or zigzag patterns (different from PVD flashes)
- “Heat wave” or shimmering effects
- Kaleidoscope-like patterns
- Binocular symptoms (affecting both eyes simultaneously)
- Symptoms lasting 10-20 minutes, typically preceding a headache
- Complete resolution after 30 minutes or less
Key differences from PVD-related flashes:
- PVD flashes are brief, sudden streaks of light
- Usually unilateral (one eye)
- Occurring intermittently over weeks or months
- Not associated with headaches
If you’re unsure whether your symptoms are migraine-related, it’s always safer to have an eye examination to rule out retinal issues.
What to Expect: The Eye Examination
When you visit an eye care provider for floaters and flashes, a thorough examination is essential to rule out retinal tears or detachment.
Comprehensive Dilated Eye Exam
Your ophthalmologist will:
1. Dilate Your Pupils Special drops widen your pupils, allowing examination of the entire retina, including the peripheral areas where tears most commonly occur.
2. Use Specialized Equipment:
- Ophthalmoscope to examine the retina directly
- Indirect ophthalmoscopy for wide-field retinal viewing
- Scleral depression (gentle pressure on the eyelid) to visualize the far peripheral retina
- Contact lens biomicroscopy for detailed retinal examination
3. Check for Warning Signs:
- Retinal tears or holes
- Vitreous hemorrhage (blood in the eye)
- Vitreous pigment (“tobacco dust”)
- Retinal detachment
- Areas of retinal thinning or lattice degeneration
Additional Diagnostic Testing
If needed, your doctor may order:
- Optical Coherence Tomography (OCT): High-resolution cross-sectional images of retinal layers
- Ultrasound of the Eye: When blood or dense floaters obscure the retina
- Fluorescein Angiography: To assess retinal blood flow and detect leaks
- Widefield Imaging: To capture images of the peripheral retina
After the exam: Your pupils will remain dilated for 4-6 hours. You may be light-sensitive and experience blurred vision. Arrange transportation if possible, as driving may be difficult.
Treatment Options: From Observation to Surgery
Treatment for floaters and flashes depends entirely on the underlying cause.
Uncomplicated PVD (No Retinal Tear)
For benign PVD without complications:
- Observation and Monitoring: Most cases require no treatment
- Follow-up Exam: Recheck at 6 weeks to detect any late-developing tears
- Patient Education: Understanding warning signs to watch for
- Brain Adaptation: Over time, most people notice floaters less as the brain learns to ignore them
Retinal Tears
When a tear is detected early:
Laser Photocoagulation:
- Quick, often painless in-office procedure
- Creates small burns around the tear
- Forms scar tissue that seals the tear
- Prevents fluid from getting under the retina
- Highly effective at preventing detachment when caught early
- Typical recovery time: a few days
- Success rate: Over 90% when performed promptly
Cryotherapy (Freezing Treatment):
- Alternative to laser for certain tear locations
- Freezes tissue around the tear
- Creates adhesion that seals the tear
- May be used when laser is not suitable
Retinal Detachment
If detachment has already occurred, surgery is required:
Pneumatic Retinopexy:
- Gas bubble injected into the eye
- Patient maintains specific head positioning for several days
- Gas bubble pushes retina back into place
- Laser or cryotherapy seals the tear
- Least invasive surgical option
- Best for certain types of detachments
Scleral Buckle:
- Silicone band sewn around the outside of the eye
- Gently pushes the eye wall inward
- Closes the tear and reattaches the retina
- Band remains permanently
- Time-tested technique with excellent outcomes
Vitrectomy:
- Surgical removal of vitreous gel
- Replaced with gas bubble or silicone oil
- Direct repair of retinal tears
- Most comprehensive approach for complex cases
- May be combined with scleral buckle
Success Rates:
- When treated promptly, 87-95% of retinal detachments can be successfully reattached with a single surgery
- Approaching 100% final success rate after one or more surgical procedures
- Best outcomes occur when treatment is received within 24-48 hours
- Delayed treatment significantly reduces success rates and visual recovery potential
Treatment for Bothersome Floaters
For people with chronic, bothersome floaters that interfere with vision and quality of life:
YAG Laser Vitreolysis
- Non-invasive laser procedure
- Breaks up larger floaters into smaller, less noticeable pieces
- Best for specific, well-defined floaters
- Not suitable for all floater types
- Mixed success rates; more research needed
- Low risk but results vary by individual
Vitrectomy for Floaters
- Surgical removal and replacement of vitreous
- Reserved for severe, debilitating floaters that significantly impact daily life
- Carries surgical risks: retinal detachment (1-2%), cataracts, infection
- Most ophthalmologists recommend this only as a last resort
- Very effective when performed, with high patient satisfaction
When to Seek Care: Your Action Plan
Understanding when to seek care can save your vision.
SAME-DAY EMERGENCY (Call Immediately or Go to ER):
- Sudden shower of new floaters
- Persistent, repeated flashes
- Dark curtain or shadow in your vision
- Sudden vision loss or significant reduction
- Any visual field defects
- Grey “curtain” moving across your vision
Action: Call West Broward Eyecare Associates immediately or go to the nearest emergency room.
WITHIN 24 HOURS (Call Your Eye Doctor Urgently):
- Subjective reduction in vision quality
- New onset of floaters with flashes
- Blood visible in your vision (vitreous hemorrhage)
- Single large new floater that appeared suddenly
Action: Contact our office for an urgent same-day or next-day appointment.
WITHIN ONE WEEK (Schedule Prompt Appointment):
- New floaters without visual field defects
- First-time floaters or flashes
- Gradual increase in floaters
Action: Schedule an appointment for a comprehensive dilated eye exam.
ROUTINE FOLLOW-UP:
- Chronic, stable floaters that haven’t changed
- Floaters you’ve had for years without progression
Action: Mention at your next regular eye exam.
Recent Research: What Science Tells Us
Study 1: Risk Assessment for Retinal Complications
A comprehensive 2009 meta-analysis published in JAMA examined nearly 200 studies involving thousands of patients presenting with acute-onset floaters and flashes.
Key findings:
- 14% of patients with acute PVD developed retinal tears
- Subjective visual reduction increased tear risk 5-fold
- Vitreous hemorrhage increased risk 10-fold
- Vitreous pigment increased risk 44-fold
- One in seven patients with sudden floaters or flashes had a retinal tear or detachment
Clinical Significance: This landmark study established the evidence base for urgent same-day referral guidelines that are now standard medical practice worldwide.
Study 2: Follow-Up Necessity After PVD
A 2017 study published in Clinical Ophthalmology examined 426 patients presenting with flashes and floaters to determine the value of follow-up examinations.
Key findings:
- 14.5% developed retinal tears
- 22.7% had vitreous or retinal hemorrhage
- Visual impairment, hemorrhage at examination, and symptom duration <24 hours were strong predictors
- Even patients presenting with floaters alone harbored a significant percentage of retinal breaks
Clinical Significance: This research justified the current standard of care requiring follow-up examinations at 6 weeks, as a small but significant percentage of retinal tears develop after the initial presentation.
Study 3: Age-Related Vitreous Changes
Recent research published in 2023 in Frontiers in Neuroscience examined the molecular and genetic pathogenesis of vitreous aging.
Key findings:
- Documented the progressive liquefaction of vitreous with age
- Identified specific protein changes that lead to floater formation
- Established that PVD prevalence increases dramatically with age (24% at 50-59 years to 87% over age 80)
- Confirmed that acute-onset floaters and flashes represent a medical emergency requiring same-day ophthalmologic evaluation
Clinical Significance: Understanding the biological mechanisms behind vitreous aging helps predict risk and improve patient education about this common condition.
Living With Floaters: Practical Coping Strategies
For people with chronic, benign floaters that don’t require treatment:
Visual Strategies
- Eye Movement Technique: Gently move your eyes up and down, then side to side to shift floaters temporarily out of your central vision
- Lighting Adjustments: Reduce bright overhead lighting; use indirect, softer light sources
- Screen Modifications: Adjust monitor brightness and use blue light filters
- Sunglasses: Wear them outdoors to reduce contrast that makes floaters more noticeable
- Background Colors: Use darker backgrounds on computers and phones to minimize floater visibility
Psychological Adaptation
- Understanding: Knowledge that floaters are harmless reduces anxiety
- Distraction: Engage in absorbing activities to shift focus away from floaters
- Patience: The brain’s natural adaptation process takes time but usually reduces awareness significantly
- Support: Consider connecting with others who experience floaters through support communities
- Acceptance: Most people find floaters become less bothersome over weeks to months
Prevention: Can You Reduce Your Risk?
While you can’t prevent natural aging of the vitreous, you can reduce risk factors for complications:
Protective Measures:
- Wear protective eyewear during sports and high-risk activities
- Maintain good control of diabetes and blood pressure
- Attend regular comprehensive eye examinations, especially if you’re at higher risk
- Report any sudden changes in vision immediately
- Follow up as recommended after PVD diagnosis
- Protect eyes from UV damage with quality sunglasses
For High-Risk Individuals:
- More frequent eye examinations (discuss appropriate schedule with your eye doctor)
- Immediate evaluation of any new symptoms
- Careful monitoring of the fellow eye if one eye has experienced PVD or complications
- Consider prophylactic laser treatment if lattice degeneration is present
Special Considerations: Floaters and Flashes in Different Populations
Children and Young Adults
While less common, floaters and flashes can occur in younger individuals:
- Often related to high myopia
- May indicate inflammatory conditions
- Always warrant thorough evaluation
- Rarely due to normal aging processes
- Higher likelihood of retinal tears in young myopes
Diabetic Patients
People with diabetes face additional risks:
- Higher risk of vitreous hemorrhage
- Diabetic retinopathy can cause similar symptoms
- More frequent monitoring essential
- Any sudden changes require urgent evaluation
- Blood sugar control is crucial for eye health
Post-Surgical Patients
After cataract surgery or other eye procedures:
- Slightly higher PVD risk
- Similar warning signs apply
- Maintain regular post-operative follow-ups
- Don’t assume all symptoms are “normal” recovery
- Report any new floaters or flashes to your surgeon
Athletes and Active Individuals
If you participate in contact sports or high-impact activities:
- Higher risk of traumatic retinal tears
- Protective eyewear is essential
- Report any eye injuries immediately
- Consider baseline retinal examination
- Know the warning signs and seek prompt care
References and Resources
This article is based on current medical research and clinical guidelines. Below are key scientific resources that informed this comprehensive guide:
Primary Research Sources:
- Hollands, H., Johnson, D., Brox, A.C., et al. (2009). “Acute-onset floaters and flashes: Is this patient at risk for retinal detachment?” JAMA, 302(20):2243-9.
https://pubmed.ncbi.nlm.nih.gov/19934426/
This landmark meta-analysis of nearly 200 studies established evidence-based guidelines for urgent referral, showing that 14% of patients with acute PVD develop retinal tears and identifying key risk factors including visual field defects and vitreous hemorrhage. - Bond-Taylor, M., Jakobsson, G., & Zetterberg, M. (2017). “Posterior vitreous detachment – prevalence of and risk factors for retinal tears.” Clinical Ophthalmology, 11:1689-1695.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5609787/
This comprehensive study of 426 patients found that 14.5% developed retinal tears, with the highest risk occurring within the first 24 hours of symptoms. The research identified visual impairment and vitreous hemorrhage as the strongest predictors of retinal complications. - Sebag, J. (2023). “Ageing of the vitreous: From acute onset floaters and flashes to retinal detachment.” Frontiers in Neuroscience, 17:1227081.
https://pubmed.ncbi.nlm.nih.gov/25841656/
Recent research examining the molecular and genetic pathogenesis of vitreous aging, confirming that PVD prevalence increases from 24% at ages 50-59 to 87% over age 80, and establishing that acute-onset symptoms represent a medical emergency requiring same-day evaluation.
For More Information:
- American Academy of Ophthalmology: https://www.aao.org/eye-health/diseases/what-are-floaters-flashes
- National Eye Institute: https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/floaters
The Bottom Line: Trust Your Instincts, Protect Your Vision
Floaters and flashes are incredibly common—most people will experience them at some point in their lives. While the vast majority of cases are benign, the potential for vision-threatening complications means that sudden changes should never be ignored.
Key Takeaways:
- Most floaters and flashes are harmless signs of natural aging
- Sudden onset or dramatic increase requires immediate evaluation within 24 hours
- Visual field changes, curtain effects, or vision loss are emergencies—seek same-day care
- Early detection and treatment of retinal tears can save your vision
- Follow-up care is essential—even uncomplicated PVD requires monitoring
- When in doubt, get checked out—it’s always better to be safe than sorry with your vision
Remember: Your eyes don’t have pain receptors in the retina, so retinal tears and early detachment are painless. Don’t wait for pain to seek care—pay attention to visual changes.
Your Vision Is Precious: Take Action Today
At West Broward Eyecare Associates, we understand how concerning sudden changes in your vision can be. As your trusted vision guardians serving the Tamarac community and surrounding areas, we’re here to provide expert care when you need it most.
Why Choose West Broward Eyecare Associates?
- Same-Day Emergency Appointments for urgent floaters and flashes
- Advanced Diagnostic Technology for comprehensive retinal examination
- Experienced Retinal Specialists trained in detecting and treating retinal conditions
- Family-Centered Care from pediatric to senior patients
- Convenient Tamarac Location serving West Broward County
- Most Insurance Plans Accepted including Medicare and Medicaid
Don’t wait. Your vision deserves the best care—and we’re here to protect it for life.
West Broward Eyecare Associates: Contact us for urgent evaluation of floaters and flashes
FAQs
-
Floaters are tiny spots or threads drifting in your vision. Flashes are brief light bursts. Both can be normal but may also signal retinal problems requiring urgent check-up.