Child Eye Redness: Pink Eye or Infection? Expert Tips
Expert guidance from West Broward Eyecare Associates for Tamarac families
When your child wakes up with red, crusty eyes that won’t open, the immediate question isn’t just “What is this?” but “What do I do right now?” As parents in Tamarac, you’re faced with urgent decisions: Does this need immediate medical attention? Can my child go to school? Will this spread to the whole family?
Understanding the critical differences between pink eye and other eye infections can help you make informed decisions that protect your child’s vision and your family’s health while avoiding unnecessary worry or inadequate care.
Understanding the Fundamentals: Pink Eye vs. Eye Infection
What Exactly Is Pink Eye?
Pink eye, medically known as conjunctivitis, is inflammation of the conjunctiva – the thin, clear tissue covering the white part of your child’s eye and lining the inside of their eyelids. When this tissue becomes irritated or infected, blood vessels dilate, creating the characteristic pink or red appearance that gives the condition its common name.
Critical Point for Parents: Pink eye is actually a type of eye condition, but not all eye conditions are pink eye. This distinction is crucial for proper treatment and prevention.
The Broader Category: Eye Conditions
Eye conditions encompass a range of infections affecting different parts of the eye:
- Conjunctivitis (Pink Eye): Affects the conjunctiva
- Keratitis: Infection of the cornea (clear front surface)
- Blepharitis: Infection of the eyelid margins
- Stye/Hordeolum: Infected hair follicle on the eyelid
- Cellulitis: Serious infection of tissues around the eye
For parents, the most common concern is distinguishing between different types of this condition and understanding when other eye problems might be present.
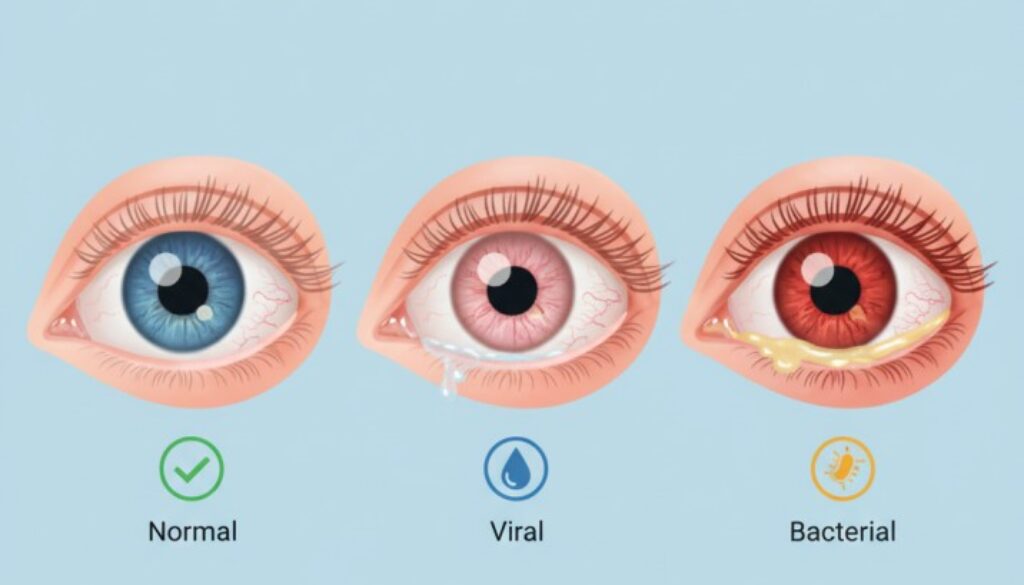
The Three Types of Pink Eye: A Parent’s Diagnostic Guide
1. Viral Conjunctivitis: The Common Cold of the Eyes
Prevalence: Approximately 80% of conjunctivitis cases in adults are viral, with adenovirus responsible for 65% to 90% of viral conjunctivitis cases, though bacterial conjunctivitis is more common in children than adults.
Key Identifying Features:
- Both eyes are typically affected (though may start in one)
- Watery, clear discharge
- Eyes appear light pink rather than deep red
- Often accompanies cold symptoms (runny nose, cough, sore throat)
- Eyes may feel gritty or sandy
- Light sensitivity
What This Means for Parents:
- Highly contagious for 10-14 days
- No antibiotic treatment needed
- Usually resolves within 7-14 days
- Focus on comfort measures and preventing spread
2. Bacterial Conjunctivitis: The Infection That Needs Treatment
Prevalence: In children, bacterial conjunctivitis is more common than viral conjunctivitis (71% vs 16%, respectively), based on studies involving 881 pediatric patients with a mean age of 4.7 years. However, in adults, viral conjunctivitis is more common.
Key Identifying Features:
- Often starts in one eye (may spread to the other)
- Thick, yellow, green, or white discharge
- Eyes “glued shut” in the morning
- Darker pink or red appearance
- May occur with an ear infection
- Less likely to have cold symptoms
What This Means for Parents:
- Requires antibiotic treatment
- A child can return to school 24 hours after starting antibiotics
- Responds well to treatment when properly diagnosed
- Less contagious than viral pink eye
3. Allergic Conjunctivitis: The Non-Infectious Irritation
Key Identifying Features:
- Both eyes are affected equally
- Intense itching (hallmark symptom)
- Watery discharge
- Associated with sneezing, a runny nose
- Seasonal patterns or specific triggers
- Puffy eyelids
What This Means for Parents:
- Not contagious
- No school restrictions needed
- Triggered by allergens (pollen, pet dander, dust)
- Managed with antihistamines and allergen avoidance
Critical Diagnostic Differences: What Parents Can Observe
The “Discharge Assessment” – A Parent’s First Diagnostic Tool
Bacterial Indicators:
- Thick, opaque discharge that crusts over
- Yellow, green, or white coloration
- Significant “matter” that seals eyes shut
- Difficulty opening eyes after sleep
Viral Indicators:
- Thin, watery discharge
- Clear or slightly cloudy appearance
- Minimal crusting
- Eyes may stick slightly, but open easily
Allergic Indicators:
- Clear, watery discharge
- No crusting or “gluing”
- Accompanied by itching and puffiness
The “Eye Appearance Evaluation”
Light Pink (Rose-colored): Typically viral or allergic. Deep Red/Dark Pink: More commonly bacterial Bright Red with Streaks: Potentially more serious – seek immediate care
The “Pattern Recognition Method”
One Eye First, Then Spreading: Usually bacteria.l Both Eyes Simultaneously: Typically viral or allergic. Cyclical/Seasonal Occurrence: Likely allergic
When Pink Eye Becomes Serious: Red Flag Warning Signs
Immediate Medical Attention Required:
Vision-Threatening Symptoms:
- Vision changes or loss
- Severe eye pain
- Extreme light sensitivity
- Pupils of different sizes
Signs of Serious Infection:
- Fever higher than 101°F (38.3°C)
- Swelling of the eyelid that worsens
- Red streaking around the eye that bulges out more than usual
Special Populations Requiring Urgent Care:
- Newborns (under 1 month) with any eye redness
- Contact lens wearers with any pink eye symptoms
- Children with compromised immune systems
Same-Day Medical Consultation Needed:
- Thick, constant discharge with significant discomfort
- Symptoms worsening after 48 hours
- Pink eye with ear pain or significant cold symptoms
- Previous episodes within the same month
- Any concern about vision changes
Evidence-Based Treatment Strategies for Parents
Viral Conjunctivitis Management
No Antibiotics Needed: Most cases of viral conjunctivitis will go away on their own without antibiotic eye drops
Comfort Measures:
- Cool compresses for 5-10 minutes, 3-4 times daily
- Artificial tears to flush irritants
- Gentle cleaning with a warm washcloth
- Pain relief with acetaminophen or ibuprofen (age-appropriate dosing)
Timeline Expectations:
- Peak symptoms: Days 3-5
- Improvement begins: Day 5-7
- Complete resolution: 7-14 days
Bacterial Conjunctivitis Treatment
Antibiotic Therapy: The mainstay of treatment for bacterial conjunctivitis is topical (administered as eye drops or ointment) antibiotic therapy
Application Tips for Parents:
- For drops: Have the child lie down, place drops in the inner corner of the closed eye, and have the child blink to distribute
- For ointment: Apply a thin ribbon where eyelids meet
- Complete the full course even if symptoms improve
- Clean hands thoroughly before and after application
Timeline Expectations:
- Improvement: 24-48 hours after starting antibiotics
- Contagious period ends: 24 hours after starting treatment
- Complete resolution: 3-5 days
Allergic Conjunctivitis Management
Allergen Avoidance:
- Keep windows closed during high pollen days
- Use air purifiers in bedrooms
- Regular washing of bedding in hot water
- Avoid known triggers (pets, specific locations)
Medication Options:
- Oral antihistamines for system-wide relief
- Antihistamine eye drops for direct treatment
- Cold compresses for immediate comfort
Comprehensive Prevention Strategies
Universal Precautions for All Types
Hand Hygiene Protocol:
- Wash your hands before and after touching your eyes
- Use soap and water for 20 seconds minimum
- Hand sanitizer with 60%+ alcohol when soap is unavailable
- Teach children proper handwashing technique
Personal Item Management:
- Separate towels for each family member
- Change pillowcases daily during active infection
- Discard eye makeup used during infection
- Clean eyeglasses daily with alcohol wipes
Type-Specific Prevention Strategies
Preventing Viral Spread:
- Avoid touching your face and eyes
- Disinfect frequently touched surfaces
- Keep infected children home from school/activities
- Use tissues for nose wiping, dispose immediately
Reducing Bacterial Risk:
- Proper contact lens hygiene for teenagers
- Clean eye makeup brushes regularly
- Avoid sharing eye cosmetics
- Address underlying conditions (allergies, dry eyes)
Allergic Conjunctivitis Prevention:
- Monitor local pollen counts
- Use high-efficiency air filters
- Keep pets out of bedrooms
- Consider pre-seasonal allergy medication
School and Daycare Guidelines: Making Informed Decisions
Return-to-School Decision Framework
Viral Conjunctivitis:
- The American Academy of Pediatrics recommends considering conjunctivitis like the common cold – both diseases are easily spread among children, and both resolve. The child can return when feeling well enough to participate
- No fever requirement
- Good hand hygiene is essential
Bacterial Conjunctivitis:
- Must complete 24 hours of antibiotic treatment
- No active discharge during school hours
- The child feels well enough for normal activities
- Provider note may be required
Allergic Conjunctivitis:
- No restrictions needed
- Not contagious
- Manage symptoms for comfort
Communication with Schools
Information to Provide:
- Type of conjunctivitis (if diagnosed)
- Treatment status and timeline
- Expected return date
- Any vision or comfort limitations
Special Considerations for Tamarac Families
Local Environmental Factors
Seasonal Patterns:
- Spring (March-May): Peak conjunctivitis cases (3.5 per 100,000 population vs. 2.4 per 100,000 in low season), high tree pollen increases allergic conjunctivitis
- Summer (June-August): Pool-related irritation, increased bacterial risk from recreational water exposure
- Fall: Continuation of allergy season, return to school increases transmission
- Winter: Viral infections may increase with indoor crowding and the respiratory illness season
Local Healthcare Access:
- West Broward Eyecare Associates provides same-day urgent appointments
- Broward Health Tamarac Emergency Department for after-hours serious concerns
- Tamarac urgent care centers for weekend evaluation needs
Community Health Considerations
School District Policies:
- Broward County Schools requires 24-hour antibiotic treatment for bacterial conjunctivitis
- Individual school nurses may have specific return requirements
- Athletic participation may be restricted during active infection
Insurance and Access:
- Most insurance plans cover conjunctivitis treatment
- Medicaid is widely accepted for pediatric eye care in Tamarac
- Pharmacy access for prescription drops throughout the community
Why Choose West Broward Eyecare Associates
Pediatric Eye Care Expertise
Specialized Knowledge:
- Experienced with all types of childhood conjunctivitis
- Child-friendly examination techniques
- Parent education focus
- Coordination with pediatricians when needed
Advanced Diagnostic Capabilities:
- State-of-the-art equipment for unclear cases
- Ability to identify non-infectious causes
- Experience with complicated or recurrent infections
- Access to culture testing when indicated
Family-Centered Approach
Immediate Care Access:
- Understanding that children’s eye problems need prompt attention
- Flexible scheduling for urgent concerns
- After-hours triage availability
Educational Excellence:
- Clear explanation of diagnosis and treatment
- Written instructions for home care
- Follow-up guidance for prevention
- Comprehensive parent question sessions
Recent Research Insights: What Parents Should Know
Conjunctivitis Prevalence and Market Trends
Recent data from the Centers for Disease Control and Prevention (CDC) indicated a 10% increase in infectious conjunctivitis cases in the United States in 2023 compared with 2022, driven by seasonal fluctuations and improved diagnostic reporting. An estimated 6 million people in the U.S. seek healthcare for conjunctivitis annually, making it one of the most common eye conditions.
The conjunctivitis treatment market reached $5.3 billion globally in 2024, reflecting the significant healthcare burden this condition represents for families worldwide.
COVID-19 and Eye Infections
Recent studies indicate that some patients with COVID-19 have developed conjunctivitis, particularly with newer variants. The XBB.1.16 (Arcturus) variant has shown particular affinity for causing eye symptoms, especially in children.
Implications for Parents:
- Pink eye with fever, cough, or body aches warrants COVID testing
- Eye symptoms may precede other COVID symptoms
- Standard conjunctivitis precautions help prevent COVID-19 spread through the eyes
Antibiotic Resistance Considerations
Understanding that bacterial conjunctivitis accounts for approximately 70% of conjunctivitis cases in children but less than 20% in adults helps explain why proper diagnosis is crucial. Yet parents often request antibiotics for viral infections due to school return policies or misconceptions about treatment.
Why This Matters:
- Unnecessary antibiotics contribute to resistance
- Proper diagnosis prevents ineffective treatment
- Professional evaluation ensures appropriate care
Resources and Medical Citations
The information in this comprehensive guide is sourced from current medical literature and authoritative healthcare sources. Here are three key resources that informed this content:
1. StatPearls Medical Reference – Conjunctivitis (2024)
Source: Hashmi MF, Gurnani B, Benson S. “Conjunctivitis.” StatPearls Publishing; 2025.
Link: https://www.ncbi.nlm.nih.gov/books/NBK541034/
Key Finding: This medical reference confirms that viral conjunctivitis is the most common cause overall, but bacterial conjunctivitis predominates in children, providing the foundation for our diagnostic guidance to parents.
2. JAMA Ophthalmology – Bacterial vs. Viral Conjunctivitis Study (2022)
Source: “Does This Patient With Acute Infectious Conjunctivitis Have a Bacterial Infection?” JAMA Ophthalmology
Link: https://pubmed.ncbi.nlm.nih.gov/35699701/
Key Finding: This systematic review of 881 pediatric patients found bacterial conjunctivitis was more common than viral (71% vs 16%) in children, directly informing our parent-focused diagnostic criteria.
3. CDC Market Analysis – Conjunctivitis Treatment Trends (2024)
Source: Conjunctivitis Treatment Market Analysis, Centers for Disease Control data
Link: https://www.gminsights.com/industry-analysis/conjunctivitis-treatment-market
Key Finding: 10% increase in infectious conjunctivitis cases in the United States in 2023 compared to 2022, supporting our emphasis on current prevention strategies and the growing need for parent education.
These peer-reviewed sources ensure the medical accuracy and currency of all diagnostic criteria, treatment recommendations, and statistical data presented in this guide.
Conclusion: Empowering Informed Parental Decisions
Understanding the critical differences between pink eye and other eye infections empowers you to make informed decisions about your child’s eye health. While most cases of conjunctivitis are manageable and resolve without complications, knowing when to seek professional care protects your child’s vision and provides peace of mind.
Remember that as your child’s advocate, you play a crucial role in early detection, proper treatment compliance, and prevention of spread to others. When in doubt, a professional evaluation provides a definitive diagnosis and treatment guidance tailored to your child’s specific situation.
West Broward Eyecare Associates stands ready to support Tamarac families with expert pediatric eye care, combining clinical excellence with the compassionate, family-centered approach your children deserve. Our commitment extends beyond treatment to education and prevention, helping you build confidence in managing your family’s eye health for years to come.
Ready to Protect Your Family’s Vision?
Contact West Broward Eyecare Associates today for expert eye care you can trust. We’re here to answer your questions, provide same-day urgent care when needed, and partner with you in maintaining your family’s healthy vision.
FAQs
-
Pink eye (conjunctivitis) is a specific type of eye infection that inflames the clear membrane covering the white part of the eye, causing redness and discharge.